For many women, painful periods are a monthly reality. If you’re one of the millions who experience cramps, bloating, fatigue, and other symptoms during your period, you’re not alone. While some discomfort is common, the severity and causes can vary significantly from one person to another. So, why does period pain happen, and how can you manage it? In this article, we’ll break down the reasons behind painful periods, explore common conditions like endometriosis and fibroids, and discuss both natural remedies and medical treatments that can help you find relief.
Understanding Period Pain: The Basics
Period pain, also known as dysmenorrhea, is common among women in their reproductive years. It occurs when the uterus contracts to shed its lining, a process that typically happens during menstruation. While these contractions are a natural part of your body’s monthly cycle, they can lead to discomfort, especially if they’re intense or prolonged.
There are two main types of period pain: primary and secondary. Primary dysmenorrhea refers to cramps that occur without any underlying medical condition, while secondary dysmenorrhea is caused by specific conditions, such as endometriosis or fibroids, that make the pain more severe.
In this article, we’ll take a closer look at both primary and secondary dysmenorrhea and explore ways to manage period pain effectively.
Causes of Period Pain: Why Does It Happen?
1. Hormonal Changes
Hormonal fluctuations are one of the main reasons period pain occurs. During the menstrual cycle, levels of estrogen and progesterone fluctuate to prepare the body for pregnancy. If pregnancy doesn’t occur, progesterone levels drop, triggering the shedding of the uterine lining (your period). This hormonal drop can cause the uterus to contract more intensely, leading to cramping and discomfort.
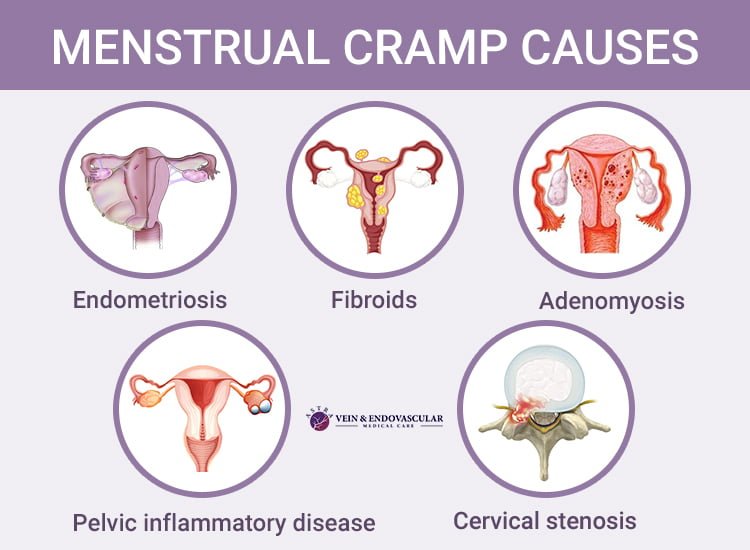
2. Endometriosis
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, often on the ovaries, fallopian tubes, and the tissue lining the pelvis. Each month, this tissue behaves like normal uterine tissue—it thickens, breaks down, and sheds. However, because the tissue is outside the uterus, it has no way to exit the body. This can lead to severe pain, especially during menstruation.
Women with endometriosis often experience debilitating cramps, heavy bleeding, and pelvic pain that can interfere with daily activities. If you have symptoms like chronic pelvic pain, painful periods, pain during intercourse, or difficulty getting pregnant, it’s essential to see a doctor for proper diagnosis and treatment. You can learn more about endometriosis from the Mayo Clinic.
3. Uterine Fibroids
Fibroids are non-cancerous growths that develop in the uterus. While many women with fibroids experience no symptoms, they can sometimes cause significant discomfort, especially during menstruation. These growths can interfere with the normal shedding of the uterine lining, leading to prolonged or heavier periods and more intense cramps.
Other symptoms of fibroids include pelvic pressure, frequent urination, and pain during sex. If you suspect you have fibroids, it’s important to consult with a healthcare provider to determine the best course of action for treatment. You can read more about fibroids and treatment options on Healthline.
4. Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease is an infection of the reproductive organs, often caused by sexually transmitted infections (STIs) such as chlamydia or gonorrhea. PID can cause pain in the lower abdomen, irregular periods, and discomfort during intercourse. Women with PID often experience chronic pelvic pain and may face difficulties conceiving if left untreated.
If you experience pain during menstruation along with symptoms like abnormal discharge or fever, it’s crucial to see a doctor for evaluation and treatment.
5. Ovarian Cysts
Ovarian cysts are fluid-filled sacs that form on the ovaries. In many cases, ovarian cysts cause no symptoms. However, when a cyst grows large enough, it can cause pain and discomfort during menstruation. The pain may be sharp or cramp-like, and some women may also experience bloating, pelvic pressure, and changes in menstrual cycles.
If an ovarian cyst ruptures or twists, it can cause intense pain and requires immediate medical attention. Regular checkups can help identify any potential cysts early on. Learn more about cysts and why they form in this article on our website.
How to Manage Period Pain: Natural Remedies and Medical Options

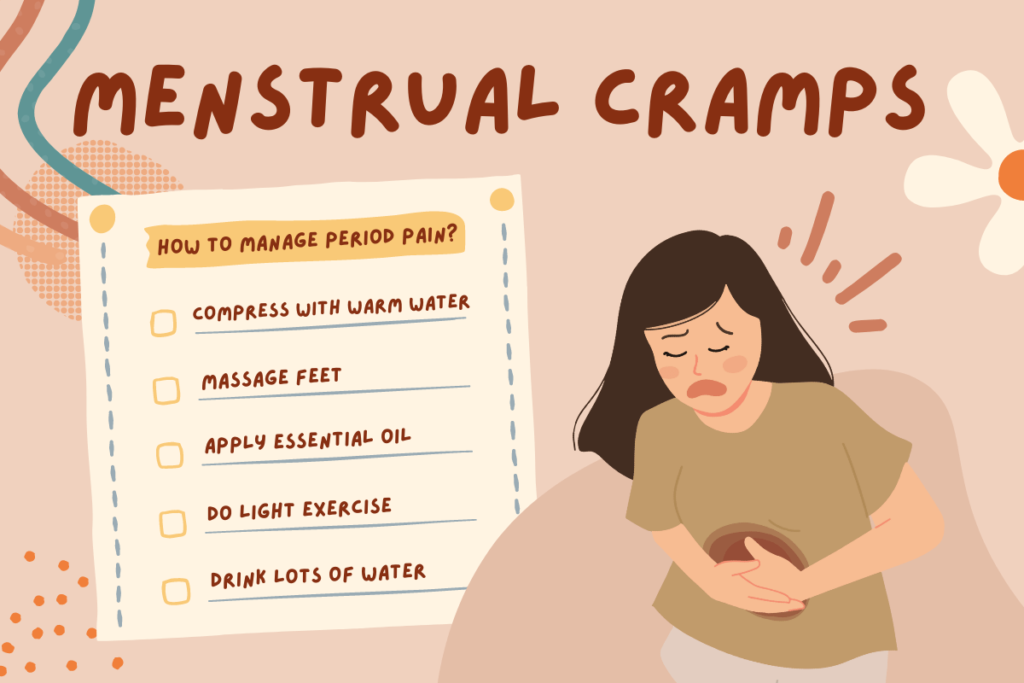
1. Heat Therapy
Heat therapy is one of the most effective natural ways to alleviate period pain. Applying heat to the lower abdomen can help relax the muscles of the uterus, reducing cramps and easing discomfort. You can use a heating pad, hot water bottle, or even a warm bath to target the painful area.
2. Exercise and Movement
It may sound counterintuitive, but physical activity can help ease period pain. Exercise releases endorphins, which are natural painkillers that help improve mood and reduce discomfort. Light exercises such as walking, yoga, or gentle stretching can help improve blood flow and reduce cramping.
3. Dietary Changes
A balanced diet can help manage period pain. Eating foods rich in magnesium, vitamin E, omega-3 fatty acids, and antioxidants can reduce inflammation and muscle tension. Some foods to consider adding to your diet include:
- Leafy greens (rich in magnesium)
- Fatty fish (such as salmon or mackerel)
- Nuts and seeds (sources of omega-3 fatty acids)
- Whole grains
- Fruits and vegetables rich in vitamin C (to combat inflammation)
Avoiding processed foods, excessive caffeine, and high-sugar snacks can also help maintain hormone balance and reduce period pain.
4. Herbal Remedies
Certain herbal remedies are known for their ability to reduce menstrual cramps. Here are a few commonly used herbs:
- Ginger: Known for its anti-inflammatory properties, ginger can help reduce pain and bloating associated with menstruation.
- Chamomile: Chamomile tea has soothing effects that can help calm the body and alleviate menstrual cramps.
- Peppermint: Peppermint oil or tea can relieve muscle tension and reduce pain.
Before trying herbal remedies, it’s important to consult with a healthcare professional, especially if you’re on medication or have underlying health conditions.
5. Over-the-Counter Pain Relievers
Over-the-counter (OTC) pain relievers, such as ibuprofen or naproxen, can be effective in reducing period pain. These nonsteroidal anti-inflammatory drugs (NSAIDs) help decrease inflammation and alleviate cramps. Make sure to follow the recommended dosage, and consult a healthcare provider if pain persists or worsens.
6. Hormonal Birth Control
Hormonal birth control methods, such as the pill, patch, or intrauterine device (IUD), can help regulate periods and reduce the severity of cramps. Birth control works by altering the hormonal fluctuations that contribute to menstrual pain, often leading to lighter, less painful periods.
Speak with your doctor about which birth control method may be best for you, as some options can provide added benefits, such as improving acne or regulating irregular cycles.
7. Surgery (For Severe Cases)
In rare cases where period pain is severe and doesn’t respond to other treatments, surgery may be considered. For example, women with endometriosis may undergo laparoscopy to remove endometrial tissue. Similarly, women with fibroids may opt for surgery to remove the growths if they’re causing significant discomfort.
Surgery is typically considered a last resort after other treatments have been exhausted.
When to See a Doctor
While occasional period pain is common, severe or persistent pain should be evaluated by a healthcare provider. If you experience any of the following symptoms, it’s time to seek medical attention:
- Severe, debilitating pain that doesn’t improve with over-the-counter pain relief
- Pain during intercourse
- Abnormal or excessively heavy periods
- Pain accompanied by fever, vomiting, or unusual discharge
- Difficulty getting pregnant
A healthcare provider can help determine the underlying cause of your period pain and recommend appropriate treatment options.
Conclusion
Understanding the causes of period pain and exploring different ways to manage it can help you regain control over your menstrual health. Whether you’re dealing with hormonal fluctuations, fibroids, endometriosis, or other underlying conditions, there are a variety of treatments available—from natural remedies to medical options. Don’t suffer in silence—take the necessary steps to improve your comfort and overall well-being during your period.
If you found this article helpful, explore more articles on women’s health and wellness or leave a comment to share your thoughts. Remember, you don’t have to manage period pain alone—help is available!