Table of Contents
Introduction
Birth control has been a cornerstone of reproductive health for decades, providing women with the freedom to manage their own fertility. With so many different methods available today, it can be overwhelming to navigate through all the options and choose the one that’s right for you. From hormonal methods like the pill and IUDs to non-hormonal options such as condoms, there is no one-size-fits-all solution.
The truth about birth control is that it’s not just about preventing pregnancy—it’s about empowering women to make informed decisions about their bodies and health. In this post, we’ll take a closer look at the most common birth control methods, how they work, their potential side effects, and how to choose the best one based on your lifestyle.
Whether you’re considering birth control for the first time or are looking to change your current method, this guide will provide you with the essential information you need to make an informed decision.
What Is Birth Control?
Birth control refers to methods or devices used to prevent pregnancy. These methods vary widely, with some focusing on preventing ovulation, while others work by blocking sperm from reaching the egg. Birth control can be divided into several categories, including hormonal and non-hormonal methods, long-term and short-term options, and emergency contraception.
Each method has its own set of benefits and drawbacks, and the best method for you will depend on your personal preferences, health history, and lifestyle.
Types of Birth Control Methods

Hormonal Methods
Hormonal birth control works by altering the natural hormonal processes in the body to prevent pregnancy. These methods typically involve either estrogen, progestin, or a combination of both hormones, which suppress ovulation, thicken cervical mucus to block sperm, and alter the lining of the uterus to prevent implantation.
- Birth Control Pills The pill is one of the most widely used methods of contraception. It contains synthetic forms of estrogen and progestin, which work together to prevent ovulation. When taken correctly, birth control pills are about 99% effective in preventing pregnancy. Pros:
- Convenient and easy to use.
- Can regulate periods and reduce menstrual cramps.
- Can improve acne in some women.
- Must be taken daily at the same time to be most effective.
- May cause side effects such as nausea, headaches, or weight gain.
- Doesn’t protect against sexually transmitted infections (STIs).
- Intrauterine Device (IUD) The IUD is a small T-shaped device inserted into the uterus by a healthcare provider. There are two main types of IUDs: hormonal and copper. Hormonal IUDs release progestin, while copper IUDs are non-hormonal and work by releasing copper ions, which create an environment that is toxic to sperm. Pros:
- Highly effective (over 99%).
- Long-lasting, with some types working for up to 5–10 years.
- Can reduce menstrual cramps and make periods lighter (for hormonal IUDs).
- Insertion can be uncomfortable, and there may be spotting for the first few months.
- May cause irregular periods or heavier periods for copper IUDs.
- Birth Control Implants Birth control implants are small rods placed under the skin of the arm. These rods release progestin, preventing ovulation and thickening cervical mucus to block sperm. The implants last for up to 3 years. Pros:
- Very effective (99% or higher).
- Long-term protection with no daily action required.
- Can lighten periods and reduce menstrual cramps.
- Requires a healthcare provider for insertion and removal.
- May cause irregular bleeding or no periods at all.
Non-Hormonal Methods
Some women prefer non-hormonal birth control methods, either due to personal health concerns or to avoid hormonal side effects. These methods focus on preventing sperm from reaching the egg.
- Condoms Condoms are a barrier method of contraception, either male or female, that prevents sperm from entering the vagina. Male condoms are worn over the penis, while female condoms are inserted into the vagina before intercourse. Pros:
- Protects against both pregnancy and sexually transmitted infections (STIs).
- Readily available and easy to use.
- Can break or slip off if not used correctly.
- Some people may have latex allergies, although non-latex options are available.
- Diaphragm A diaphragm is a flexible silicone cup that covers the cervix to prevent sperm from entering the uterus. It is typically used with spermicide to increase its effectiveness. Pros:
- Non-hormonal and does not affect menstrual cycles.
- Can be used on-demand, not requiring continuous use.
- Must be used correctly with spermicide.
- Less effective than other methods when not used properly.
Permanent Methods
For those who no longer wish to have children or are certain they don’t want to have children in the future, permanent birth control methods can offer a lifelong solution.
- Sterilization (Tubal Ligation or Vasectomy) Sterilization is a permanent form of birth control. For women, tubal ligation involves cutting or blocking the fallopian tubes, while for men, a vasectomy involves cutting the vas deferens to prevent sperm from entering the semen. Pros:
- Permanent, no need to worry about contraception again.
- Highly effective.
- Surgical procedure with risks of complications.
- Not easily reversible, so it’s important to be sure of your decision.
Birth control—once a hushed topic—is now front and center in conversations about health, relationships, and personal freedom. But despite the growing openness, misconceptions still persist. From confusing information online to well-meaning but outdated advice, many people still don’t fully understand how birth control works, what options exist, and how to make informed choices.
This guide breaks down everything you need to know about birth control in 2025—from methods and myths to side effects, benefits, and real-world impact.
Why Birth Control Matters
At its core, birth control is about reproductive autonomy—the ability to decide if, when, and how to have children. But it’s more than just a way to prevent pregnancy. Birth control can also:
- Treat medical conditions like PCOS, endometriosis, or acne
- Help regulate painful or irregular periods
- Empower women to pursue education, careers, or financial stability
- Reduce risks of unintended pregnancies and their associated emotional or economic stress
In a world where health information is widely accessible, understanding your contraceptive options is part of being informed, responsible, and proactive.
Types of Birth Control
Modern contraception comes in many forms. Some are hormonal, some are non-hormonal. Some are short-term, others long-acting. Here’s a breakdown of the most common types:
1. Hormonal Methods
These methods regulate hormones to prevent ovulation or alter the uterus lining to prevent fertilization.
- Birth Control Pills: Taken daily, they’re 91-99% effective when used correctly. Combination pills (estrogen + progestin) and progestin-only pills are both available.
- Birth Control Patch: Applied to the skin weekly. It releases estrogen and progestin.
- Vaginal Ring (e.g., NuvaRing, Annovera): Inserted monthly, it delivers hormones locally.
- Birth Control Shot (Depo-Provera): Given every 3 months. Convenient but may delay return to fertility.
- Implant (Nexplanon): A matchstick-sized rod placed under the skin of the arm. Effective for up to 3–5 years.
2. Intrauterine Devices (IUDs)
IUDs are small, T-shaped devices inserted into the uterus. Two main types:
- Hormonal IUD (e.g., Mirena, Kyleena): Releases progestin. Effective for 3–8 years.
- Copper IUD (ParaGard): Non-hormonal. Effective for up to 10–12 years. May cause heavier periods initially.
IUDs are over 99% effective and low-maintenance once inserted.
3. Barrier Methods
Physically prevent sperm from reaching the egg. Include:
- Condoms (male and female): Also protect against STIs.
- Diaphragms and Cervical Caps: Less common, used with spermicide.
- Sponge: Foam device with spermicide inserted before sex.
Barrier methods are less effective than hormonal ones (~71–88%) but are useful for back-up protection or in low-risk situations.
4. Emergency Contraception
Used after unprotected sex or contraceptive failure:
- Morning-After Pills (e.g., Plan B, Ella): Most effective within 72 hours.
- Copper IUD: Can be inserted up to 5 days after sex for 99% effectiveness.
5. Permanent Methods
For those who are done having children:
- Tubal Ligation (Women): Surgical procedure to block fallopian tubes.
- Vasectomy (Men): Blocks sperm from entering semen. Safer, quicker, and more effective than female sterilization.
Natural & Behavioral Methods
These methods avoid medical devices or hormones but are less reliable:
- Fertility Awareness (FAM): Tracking ovulation to avoid sex during fertile windows.
- Withdrawal Method (Pull-out): Very risky and prone to failure.
- Abstinence: The only 100% guaranteed method—but not realistic for everyone long-term.
Common Myths About Birth Control
Despite widespread use, myths still confuse people. Let’s clear some of them up:
Myth 1: Birth control makes you infertile.
✅ Most methods are fully reversible. Fertility usually returns quickly after stopping.
Myth 2: You don’t need birth control if you don’t have regular periods.
✅ Ovulation can still happen unexpectedly. Always use protection if avoiding pregnancy.
Myth 3: The pill causes cancer.
✅ Studies show it can reduce the risk of ovarian and endometrial cancers. Long-term use is safe for most healthy women.
Myth 4: Condoms aren’t effective.
✅ When used correctly, condoms are up to 98% effective and prevent STIs—unlike hormonal methods.
Myth 5: You can’t get pregnant while breastfeeding.
✅ Lactational Amenorrhea (LAM) only works in the first 6 months postpartum if the woman is exclusively breastfeeding and hasn’t had a period. It’s unreliable otherwise.
Side Effects: What to Expect
Different birth control methods affect people differently. Some common side effects include:
Hormonal Methods:
- Nausea or headaches (usually temporary)
- Breast tenderness
- Mood swings or depression (in some users)
- Weight fluctuations (not always related)
- Irregular bleeding, especially during the first few months
IUDs:
- Cramping or spotting post-insertion
- Heavier periods (with copper IUDs)
- Hormonal IUDs often reduce or eliminate periods
Barrier Methods:
- Latex allergy (opt for non-latex condoms)
- Reduced sensation for some users
Most side effects are mild and resolve within a few months. If not, switching methods is always an option.
Who Should Avoid Certain Methods?
While birth control is safe for most people, specific health conditions may rule out some options:
- History of blood clots or stroke: Avoid estrogen-based methods.
- Smokers over 35: Increased risk with combination pills or patches.
- Liver disease or migraines with aura: Avoid certain hormonal types.
Always consult a healthcare provider for personalized recommendations.
Benefits Beyond Birth Control
Contraception isn’t just for preventing pregnancy. Many women use birth control to:
- Regulate menstrual cycles
- Reduce acne
- Manage endometriosis or PCOS
- Treat anemia caused by heavy periods
- Control premenstrual syndrome (PMS) or PMDD
In fact, up to 58% of pill users in the U.S. also rely on it for non-contraceptive health benefits.
Birth Control and Mental Health
A growing area of research explores how hormonal birth control may affect mental health. Some users report:
- Mood changes
- Anxiety or depression symptoms
- Reduced libido
However, large-scale studies show no consistent link across the population. For some, hormonal methods stabilize mood; for others, they may worsen it. It’s important to track your symptoms and speak with your provider if you notice negative changes.
Cost and Access in 2025
Thanks to expanding telehealth, mobile clinics, and public awareness, birth control is more accessible than ever—but gaps remain.
- In the U.S.: Most health insurance plans cover contraception. Title X clinics offer free or low-cost services.
- Globally: Accessibility depends on location, income, and education. In some countries, social stigma or religious opposition still creates barriers.
New tech platforms now let users order pills or patches online, consult doctors virtually, and get discreet deliveries. Apps like Nurx, The Pill Club, and Favor are especially popular with Gen Z and millennials.
Talking to Your Partner
Birth control isn’t just a woman’s issue—it’s a shared responsibility. Whether you’re dating, in a long-term relationship, or exploring your sexuality, communication matters:
- Discuss STI prevention
- Share expectations around pregnancy and timing
- Decide who takes the lead—or share responsibility
- Be open about concerns, side effects, or past experiences
Mutual respect and informed choices create healthier, more honest relationships.
Side Effects of Birth Control
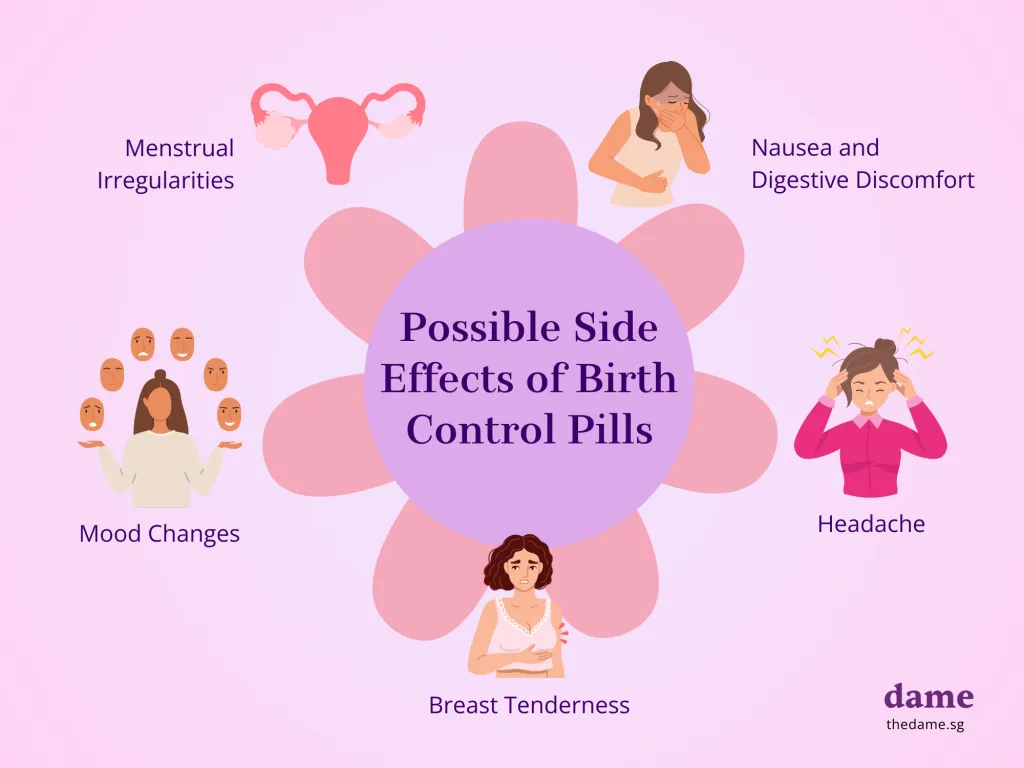
While birth control methods are highly effective at preventing pregnancy, they can also cause side effects. These side effects can vary depending on the method used and individual body reactions. Here are some common side effects associated with various birth control methods:
- Hormonal Methods: Some women may experience weight gain, mood swings, headaches, nausea, or changes in libido.
- IUDs: Hormonal IUDs can lead to lighter periods, while copper IUDs may cause heavier periods and cramping.
- Condoms: Condoms are generally safe, but some people may experience irritation or allergic reactions to latex.
It’s important to discuss any concerns with your healthcare provider to choose the right method based on your health history and lifestyle.
Choosing the Best Birth Control for Your Lifestyle
When choosing a birth control method, consider your health needs, convenience, and long-term goals. Here are some factors to consider when selecting the best method for you:
- Convenience: If you’re looking for a low-maintenance option, long-term methods like IUDs or implants may be ideal. If you prefer something that you can control daily, the pill or condoms may be a better fit.
- Health Conditions: Some methods may not be suitable for women with certain health conditions, such as those who smoke or have a history of blood clots. Always consult with your healthcare provider to determine what’s safe for you.
- Side Effects: If you’re concerned about hormonal side effects, non-hormonal methods like condoms or copper IUDs may be better suited for you.
- Future Family Plans: If you plan on having children in the future, reversible options like the pill or IUD may be preferable to permanent options like sterilization.
Conclusion: Making Informed Decisions About Birth Control
Choosing the right birth control method is a personal decision that should be based on your health, lifestyle, and reproductive goals. Each method has its own set of benefits and potential side effects, so it’s essential to weigh your options carefully. Don’t hesitate to consult your healthcare provider to discuss which birth control method is the most suitable for your needs.
Ultimately, the truth about birth control is that there’s no “one-size-fits-all” solution, but with the right information, you can make an informed decision that aligns with your health and lifestyle.
If you’re interested in learning more about reproductive health, particularly conditions like PCOS, which can affect fertility, be sure to check out PCOS: Understanding Symptoms and Effective Treatment.
Explore more articles on reproductive health and feel free to leave a comment below to share your experiences or ask questions!
Frequently Asked Questions About Birth Control
- What is birth control, and how does it work?
- Birth control refers to methods used to prevent pregnancy. It works in different ways, such as stopping ovulation, thickening cervical mucus, or altering the uterine lining to prevent fertilization or implantation.
- What are the different types of birth control available?
- There are various methods, including hormonal (pills, patches, IUDs, injections), barrier methods (condoms, diaphragms), permanent options (sterilization), and natural methods (calendar or withdrawal method).
- How effective is birth control?
- The effectiveness depends on the method used. For instance, birth control pills are about 91% effective with typical use, while an IUD can be over 99% effective.
- What are the side effects of birth control?
- Side effects can include weight changes, mood swings, headaches, nausea, or changes in menstrual cycles. However, not everyone experiences them, and they vary by individual and method used.
- Can birth control be used for reasons other than pregnancy prevention?
- Yes, many people use birth control for non-contraceptive benefits, such as managing menstrual cycles, reducing acne, or alleviating symptoms of conditions like endometriosis.
- Does birth control protect against sexually transmitted infections (STIs)?
- Most birth control methods do not protect against STIs, except for condoms. If STI protection is needed, using condoms in combination with other birth control methods is recommended.
- What should I do if I miss a birth control pill or injection?
- If you miss a pill, follow the instructions on the package. For an injection, contact your healthcare provider to determine the next steps and whether a backup method is necessary.
- Is birth control safe for everyone?
- Birth control is generally safe for most people, but some individuals may have health conditions or risk factors that require different options. It’s important to consult with a healthcare provider before choosing a method.
- Can birth control cause infertility?
- No, birth control does not cause infertility. Once you stop using birth control, your fertility typically returns to normal, although it may take some time for certain methods, like injections, to wear off.
- How do I know which birth control method is right for me?
- The best method depends on your lifestyle, health, and preferences. Consult with your doctor to discuss the pros and cons of each option, including effectiveness, side effects, and convenience.