Table of Contents
Understanding Lupus: A Chronic Disease That Affects Women’s Health
Lupus is a chronic and often misunderstood autoimmune disease that affects millions of people worldwide. In the case of lupus, the body’s immune system, which is meant to protect against infections and diseases, mistakenly attacks its own tissues, resulting in widespread inflammation and damage. This can affect multiple organs such as the skin, joints, kidneys, heart, and lungs. While lupus can affect both men and women, it disproportionately impacts women, especially those of reproductive age.
Approximately 9 out of 10 individuals diagnosed with lupus are women, and the majority of cases occur in women aged 15 to 45. This makes lupus a critical health issue for women, and it is important to understand how this chronic condition specifically affects women’s health. In this article, we will explore the unique aspects of lupus in women, its symptoms, diagnostic challenges, treatment options, and lifestyle changes that can help manage the disease.
What is Lupus?

Lupus is an autoimmune disease in which the body’s immune system mistakenly targets its own tissues and organs. Normally, the immune system defends against harmful pathogens such as viruses, bacteria, and other invaders. However, in lupus, the immune system attacks healthy tissues, leading to inflammation, pain, and damage to various organs. This inflammation can occur in different parts of the body, including the skin, joints, kidneys, heart, and lungs.
The most common form of lupus is Systemic Lupus Erythematosus (SLE), which can affect multiple organs and systems. There are other forms of lupus, including Discoid Lupus Erythematosus, which primarily affects the skin, and Drug-Induced Lupus, which is caused by certain medications. Lupus is a chronic disease, meaning that it persists for a long time, often for a person’s entire life, and it tends to flare up periodically.
How Lupus Affects Women Differently
Lupus is significantly more prevalent in women than in men, with approximately 90% of lupus patients being women. The reasons for this gender disparity are not fully understood, but it is believed that hormonal, genetic, and environmental factors contribute to the higher prevalence in women. Hormonal fluctuations, particularly the role of estrogen, are believed to play a crucial role in the development and progression of lupus in women.
The Role of Estrogen
Estrogen, the primary female sex hormone, is thought to influence the immune system in a way that may increase the risk of autoimmune diseases like lupus. In women, estrogen can increase the activity of certain immune cells, which may lead to the immune system attacking the body’s tissues more aggressively. This might explain why lupus often develops during the reproductive years when estrogen levels fluctuate.
Moreover, the severity of lupus symptoms can vary based on a woman’s menstrual cycle, pregnancy, and menopause. Hormonal changes during pregnancy may cause the disease to flare up, whereas menopause can affect how the disease progresses.
Lupus and Reproductive Health
For women with lupus, reproductive health is an area of concern. Lupus can affect pregnancy, fertility, and menstruation. While many women with lupus are able to have children, the disease can increase the risk of complications such as preterm birth, miscarriage, and high blood pressure during pregnancy.
Managing lupus during pregnancy requires careful planning and coordination between the patient and healthcare provider. Women with lupus who are considering pregnancy should be closely monitored, particularly to avoid flares during pregnancy and to ensure kidney function remains stable, as lupus can significantly affect kidney health.
Common Symptoms of Lupus in Women
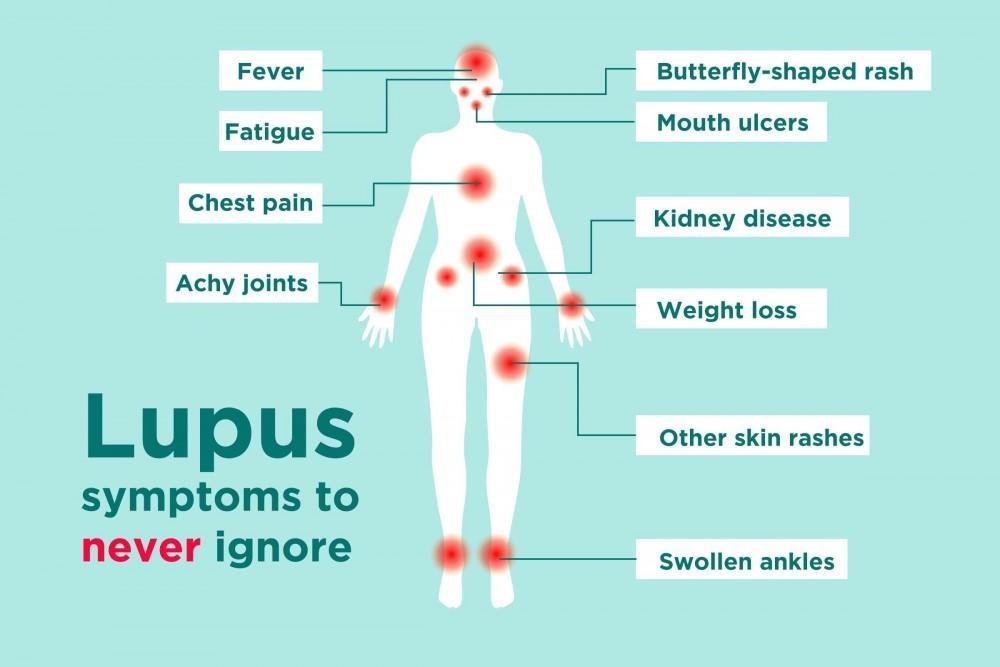
Lupus is often referred to as “the great imitator” because its symptoms can resemble those of other diseases, making it difficult to diagnose. The symptoms of lupus vary from person to person, and they may come and go, often referred to as “flares” and “remissions”. However, there are certain hallmark symptoms that are commonly seen in women with lupus.
1. Chronic Fatigue
Fatigue is one of the most common and debilitating symptoms of lupus. Women with lupus often experience persistent tiredness that is not relieved by rest. Unlike typical tiredness, lupus-related fatigue is extreme and can significantly impact daily activities. This exhaustion can make it difficult for women to perform even simple tasks, affecting their work, social life, and overall quality of life.
Fatigue in lupus can be caused by various factors, including inflammation in the body, the body’s immune response, and the side effects of medications used to treat lupus. It’s also important to note that women with lupus may experience periods of extreme fatigue during flare-ups, which can make daily functioning even more difficult.
2. Skin Rash
A hallmark symptom of lupus is a butterfly-shaped rash across the cheeks and nose, also known as the “malar rash.” This rash is often triggered by sun exposure and can appear as red, raised, and scaly patches. In addition to the malar rash, women with lupus may develop other rashes on different parts of the body, particularly on areas that are exposed to sunlight.
The rash can be one of the most visible signs of lupus, which can have a significant emotional impact on women. The malar rash is a distinctive symptom, but not everyone with lupus will experience it. It is important for women to take precautions to protect their skin from the sun, such as wearing sunscreen and protective clothing.
3. Joint Pain and Swelling
Lupus often causes inflammation in the joints, leading to pain, swelling, and stiffness. The joints most commonly affected by lupus are the fingers, wrists, and knees. Joint pain can be intermittent or chronic and can range from mild discomfort to severe pain that limits movement.
In addition to pain and swelling, lupus can cause damage to the cartilage and bones in the affected joints. Over time, this damage can result in long-term joint problems and disability if not properly managed. Joint pain can also affect a woman’s ability to perform everyday tasks, such as walking, typing, or lifting objects.
4. Hair Loss
Hair loss is another common symptom of lupus, affecting many women with the disease. Lupus-related hair loss can be caused by inflammation of the scalp or as a side effect of medications such as corticosteroids. The hair loss can be patchy or general thinning, and while it is often temporary, it can be distressing for many women.
Hair loss can have a significant emotional impact, especially for women who may already be coping with other visible symptoms such as rashes or joint pain. If you are experiencing hair loss due to lupus, it is important to talk to your healthcare provider, as there are treatments available that may help minimize or prevent further hair loss.
5. Kidney Involvement
One of the most serious complications of lupus is kidney involvement, known as lupus nephritis. This occurs when lupus causes inflammation in the kidneys, impairing their ability to filter waste from the blood. Symptoms of lupus nephritis may include swelling in the legs or feet, high blood pressure, and changes in urination (such as dark, foamy urine).
Kidney damage caused by lupus can lead to kidney failure if not properly managed. Women with lupus should undergo regular kidney function tests to monitor for any signs of kidney involvement. Early detection and treatment are essential to prevent irreversible kidney damage.
6. Chest Pain and Shortness of Breath
Inflammation of the lungs or the lining of the heart (pericarditis) is another common manifestation of lupus. This can cause chest pain and shortness of breath, which can be alarming symptoms. The inflammation can make it difficult to breathe deeply and can result in pleuritis (inflammation of the lining of the lungs) or pericarditis (inflammation of the lining around the heart).
Women with lupus should seek medical attention if they experience persistent chest pain or difficulty breathing. These symptoms may indicate a more severe complication and require prompt treatment.
How Lupus is Diagnosed
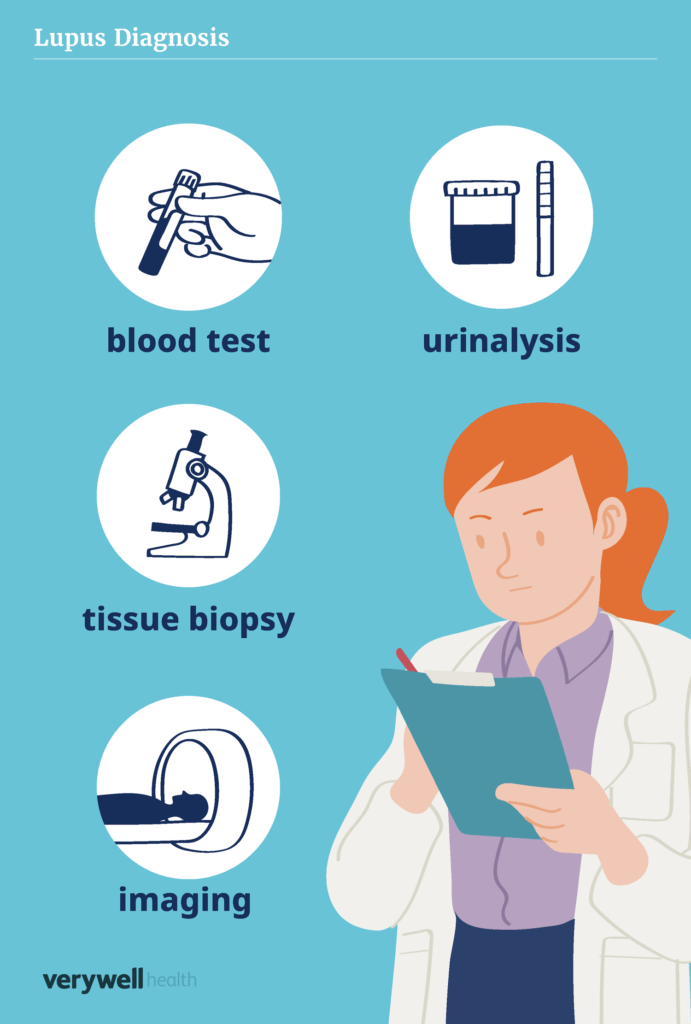
Diagnosing lupus can be challenging because its symptoms are similar to those of many other diseases. There is no single test that can definitively diagnose lupus, so doctors rely on a combination of methods to make a diagnosis. A thorough medical history, physical exam, lab tests, and sometimes imaging studies are all part of the diagnostic process.
Common Diagnostic Tools
- Blood Tests: The most common test used to diagnose lupus is a blood test that detects the presence of antibodies. The most frequently tested antibodies are antinuclear antibodies (ANA), which are often elevated in lupus patients.
- Urinalysis: Since lupus can affect the kidneys, doctors may use a urinalysis to check for abnormalities such as protein or blood in the urine, which can be signs of kidney involvement.
- Biopsy: In some cases, a biopsy of affected organs, such as the skin or kidneys, may be required to confirm the extent of damage and to determine the best course of treatment.
Treatment Options for Managing Lupus
Although there is no cure for lupus, there are various treatment options that can help manage the disease and reduce symptoms. The goal of treatment is to control inflammation, prevent flare-ups, and minimize organ damage.
1. Medications
The treatment of lupus typically involves medications to control symptoms and reduce inflammation. The choice of medication depends on the severity of lupus and which organs are affected.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These drugs help reduce joint pain, muscle aches, and inflammation caused by lupus.
- Antimalarial Drugs: Medications like hydroxychloroquine (Plaquenil) are used to treat skin rashes, joint pain, and reduce flare-ups.
- Corticosteroids: These are powerful anti-inflammatory drugs that can quickly reduce lupus symptoms, but long-term use can have significant side effects, such as weight gain and osteoporosis.
- Immunosuppressive Drugs: For more severe cases, immunosuppressive medications like cyclophosphamide or azathioprine are used to suppress the immune system and prevent it from attacking the body.
- Biologic Therapy: Belimumab (Benlysta) is a biologic drug that helps target and inhibit specific immune system components involved in lupus. This medication has shown effectiveness in reducing disease activity.
2. Lifestyle Changes and Self-Care
Lifestyle modifications are crucial in managing lupus. Key changes include:
- Sun Protection: Sun exposure can trigger lupus flare-ups, so wearing sunscreen and protective clothing is important.
- Regular Exercise: Gentle exercises such as walking, swimming, and yoga can help improve flexibility, reduce stress, and strengthen muscles.
- Dietary Adjustments: A balanced diet rich in fruits, vegetables, and lean proteins helps reduce inflammation and supports overall health.
- Stress Management: Managing stress is essential to avoid lupus flare-ups. Techniques such as meditation, mindfulness, and deep-breathing exercises can help.
- Regular Check-Ups: Routine visits to healthcare providers, especially rheumatologists, are essential for monitoring lupus symptoms and adjusting treatment plans.
3. Mental Health Support
Dealing with a chronic illness like lupus can take a toll on a woman’s mental health. Many women with lupus experience depression, anxiety, and feelings of isolation. Seeking support from mental health professionals or support groups can provide relief and improve quality of life.
For more insights on managing lupus, you can check out Healthline’s guide on lupus treatment and WebMD’s overview of living with lupus. Additionally, understanding the role of endometrial health in women’s overall well-being, including conditions like lupus, can be crucial. You may find it helpful to explore The Endometrial Microbiome: Impact on Fertility and Health for more information.
Conclusion: Embracing Life with Lupus
Lupus is a chronic disease that requires ongoing management, but with the right medical care, lifestyle adjustments, and support, women can lead fulfilling lives despite the challenges. Understanding the symptoms, seeking early treatment, and making lifestyle changes are key components in managing lupus and minimizing its impact on daily life. If you or someone you know is living with lupus, know that you are not alone, and help is available.
Explore more articles on health and wellness or leave a comment below with your experiences or questions about lupus. We’re here to help!
Frequently Asked Questions (FAQs)
1. How is lupus diagnosed in women?
Lupus is diagnosed using a combination of tests, including blood tests for antinuclear antibodies (ANA), urinalysis to check for kidney involvement, and sometimes biopsies of skin or kidneys. A thorough physical exam and medical history are also part of the diagnosis.
2. Can lupus affect fertility and pregnancy?
Lupus can affect fertility and pregnancy, but many women with lupus can conceive and have successful pregnancies with proper management. Women planning pregnancy should consult with a healthcare provider to ensure disease activity is controlled before attempting to conceive.
3. How can lupus be managed?
Lupus can be managed with medications, lifestyle changes, and regular monitoring by healthcare professionals. Medications like NSAIDs, antimalarials, and immunosuppressants are often used to control symptoms. Lifestyle changes such as sun protection, regular exercise, and stress management are also key.
4. Is lupus curable?
There is no cure for lupus at present, but the disease can be managed effectively with the right treatments. Early diagnosis and consistent management can help reduce flare-ups and prevent organ damage.
5. What are the early symptoms of lupus?
Early symptoms of lupus can include fatigue, skin rashes, joint pain, hair loss, and kidney problems. However, the symptoms vary greatly among individuals, so it’s important to consult a healthcare provider if you suspect lupus.