Table of Contents
Introduction
Polycystic Ovary Syndrome (PCOS) is a common yet often misunderstood condition that affects many women, particularly during their reproductive years. It is a hormonal disorder that can lead to a range of symptoms, such as irregular periods, acne, weight gain, and difficulty getting pregnant. Although it is not fully understood, PCOS can impact a woman’s overall health and quality of life, making early diagnosis and management crucial. In this comprehensive guide, we’ll dive deep into the symptoms of PCOS, discuss effective treatments—both medical and natural—and explore how lifestyle changes can help manage the condition.
By the end of this article, you will have a clearer understanding of PCOS and how you can take proactive steps to manage your health and well-being.
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a hormonal condition that affects approximately 1 in 10 women of reproductive age, making it one of the most common hormonal disorders among women. It is marked by an imbalance in reproductive hormones, which can lead to the growth of cysts on the ovaries, irregular periods, and issues with ovulation. While the exact cause of PCOS is still not fully known, it is often linked to genetics, insulin resistance, and inflammation.
Some of the key hormones involved in PCOS are:
- Androgens (male hormones): Women with PCOS often have higher levels of androgens, which can lead to symptoms like excess facial or body hair (hirsutism) and acne.
- Insulin: Insulin resistance, where the body does not respond to insulin effectively, is commonly seen in women with PCOS. This can lead to higher levels of insulin in the body, contributing to weight gain and an increased risk of type 2 diabetes.
Understanding PCOS is essential for managing its symptoms and seeking proper treatment.
Common Symptoms of PCOS
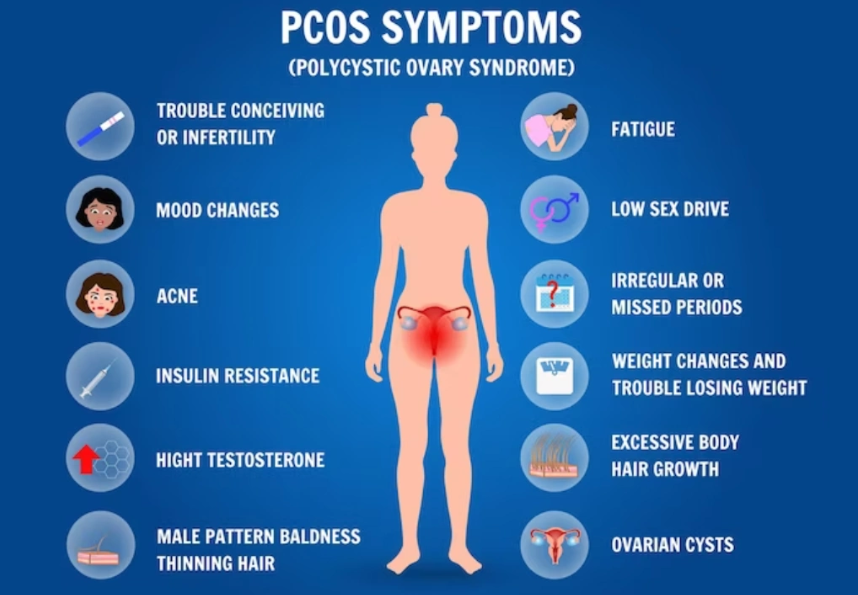
PCOS manifests in a variety of symptoms, which can vary in severity. Some women may experience only a few of the symptoms, while others may experience many. Here are some of the most common signs of PCOS:
1. Irregular Periods
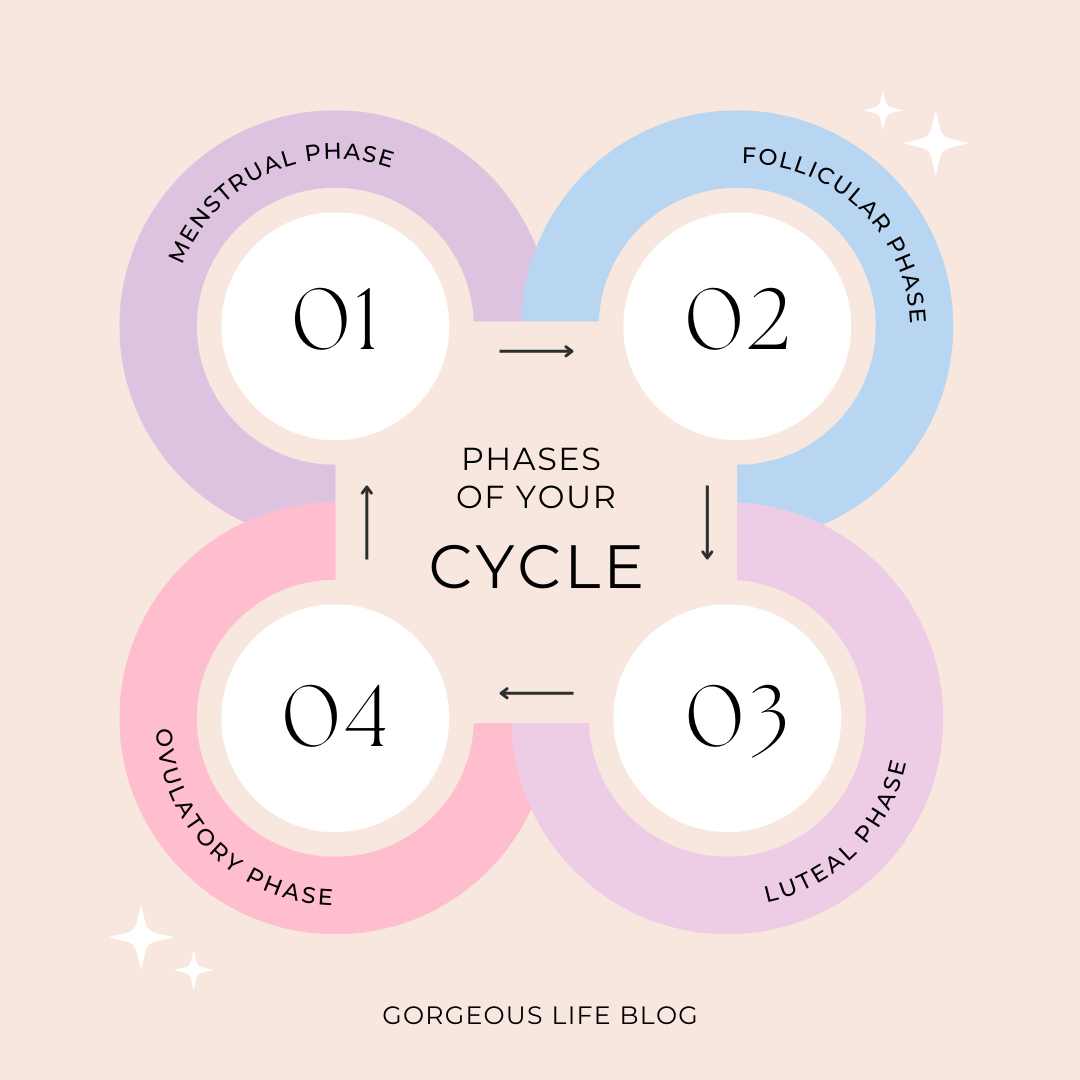
One of the hallmark signs of PCOS is irregular menstruation. Women with PCOS often experience infrequent periods (less than eight periods a year) or periods that are very heavy and prolonged. The hormonal imbalance can interfere with the normal process of ovulation, making it difficult for the body to regulate the menstrual cycle.
2. Acne and Oily Skin
Higher levels of androgens can result in an overproduction of oil, leading to acne. This can occur not only on the face but also on the chest, back, and shoulders. If you’ve noticed that your acne is persistent or severe, it could be a symptom of PCOS.
3. Weight Gain and Difficulty Losing Weight
Many women with PCOS experience weight gain, especially around the abdomen. This is often due to insulin resistance, where the body is less able to process sugar and carbohydrates, leading to fat storage. Additionally, weight loss can be particularly difficult for women with PCOS due to metabolic imbalances.
4. Excess Hair Growth (Hirsutism)
As a result of elevated androgen levels, women with PCOS may develop unwanted hair growth on the face, chest, abdomen, and back. This condition, known as hirsutism, can cause emotional distress and impact self-esteem.
5. Thinning Hair and Scalp Hair Loss
In addition to excess hair growth on the body, PCOS can also cause thinning hair or hair loss on the scalp. This is also linked to elevated androgen levels and can affect a woman’s overall appearance.
6. Infertility
PCOS is one of the leading causes of infertility in women. Since women with PCOS often do not ovulate regularly, it can be more challenging to conceive. However, with the right treatment, many women with PCOS are able to become pregnant.
7. Skin Darkening (Acanthosis Nigricans)
Some women with PCOS may notice dark patches of skin, especially in areas such as the neck, underarms, and groin. These patches are often velvety in texture and are a sign of insulin resistance.
How PCOS Affects Overall Health
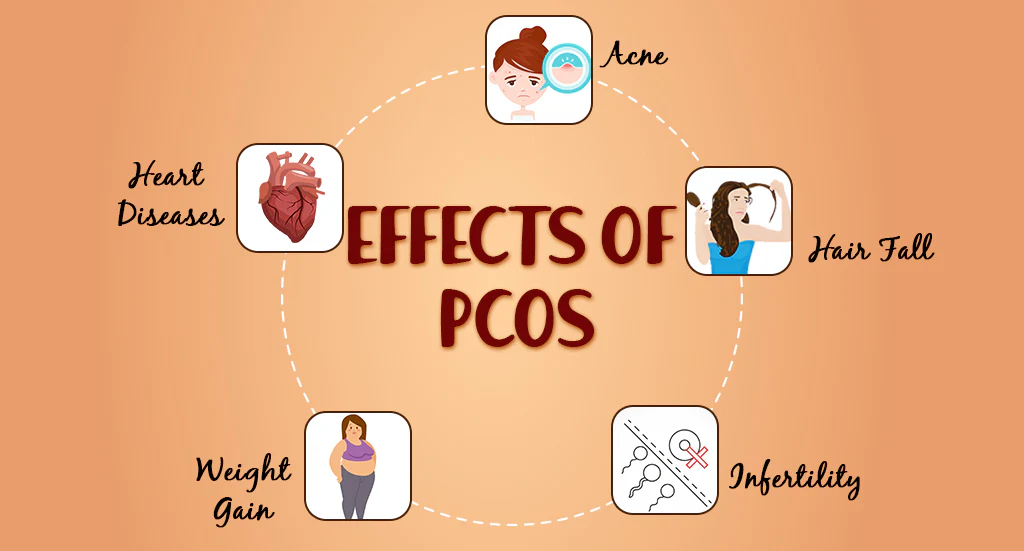
PCOS doesn’t just affect reproductive health; it can also have a long-term impact on overall health. Women with PCOS are at an increased risk for several conditions, including:
- Type 2 Diabetes: Due to insulin resistance, women with PCOS are more likely to develop type 2 diabetes.
- Heart Disease: Insulin resistance and high blood sugar levels can increase the risk of developing cardiovascular disease over time.
- Endometrial Cancer: Irregular periods and lack of ovulation can lead to a buildup of the uterine lining, which may increase the risk of endometrial cancer.
- Sleep Apnea: Women with PCOS are more likely to experience sleep apnea, especially if they are overweight.
Recognizing the long-term health risks associated with PCOS is important, as managing symptoms early can help reduce these risks.
Effective Treatments for PCOS
While there is no cure for PCOS, several treatments can help manage the symptoms and reduce the associated health risks. The treatment plan will vary depending on the severity of the symptoms and whether the woman is trying to conceive. Here are some of the most common treatments for PCOS:
Medical Treatments
- Birth Control Pills
- Oral contraceptives are often prescribed to regulate menstrual cycles, reduce acne, and manage hirsutism by lowering androgen levels. Birth control pills help balance hormones and can be an effective solution for managing symptoms.
- Metformin
- Metformin is commonly prescribed to women with PCOS who are insulin resistant. It helps lower blood sugar levels and can improve ovulation, making it easier to conceive.
- Clomiphene (Clomid)
- For women with PCOS who are struggling with infertility, clomiphene is a fertility drug that stimulates ovulation. It is one of the most common treatments for women trying to get pregnant.
- Anti-Androgen Medications
- Medications like spironolactone can help lower androgen levels, reducing symptoms such as excessive hair growth and acne.
- Progesterone Therapy
- If you have irregular periods, your doctor may recommend progesterone therapy to help regulate your menstrual cycle and reduce the risk of endometrial cancer.
Natural Treatments and Lifestyle Changes
In addition to medical treatments, certain lifestyle changes and natural remedies can help manage PCOS symptoms and improve overall health.
- Diet and Nutrition
- A balanced diet that includes whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables can help reduce insulin resistance. Avoiding processed foods and refined sugars can prevent blood sugar spikes and promote weight loss.
- Some studies suggest that a low glycemic index (GI) diet can be beneficial for women with PCOS, as it helps regulate blood sugar levels. You can read more about the connection between diet and hormonal balance in our article on hormonal imbalance causes, symptoms, and remedies.
- Exercise
- Regular physical activity can improve insulin sensitivity, help with weight loss, and reduce symptoms such as acne and hirsutism. Aim for at least 150 minutes of moderate-intensity exercise per week, such as brisk walking, swimming, or cycling.
- Herbal Remedies
- Certain herbs, such as spearmint tea, have been shown to help reduce hirsutism in women with PCOS. While more research is needed, herbal remedies can be a complementary approach to managing symptoms.
- Stress Management
- Chronic stress can exacerbate PCOS symptoms. Incorporating stress management techniques such as meditation, yoga, or mindfulness can help improve both mental and physical health.
- Supplements
- Some women with PCOS find relief by taking supplements like inositol (especially myo-inositol) and vitamin D, which may improve insulin sensitivity and menstrual regularity.
For more detailed information on how hormonal imbalances can affect your health, you can explore our guide on hormonal imbalance causes, symptoms, and remedies.
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders affecting women of reproductive age. Despite its prevalence—impacting up to 1 in 10 women globally—PCOS remains widely misunderstood and frequently underdiagnosed. Its symptoms go far beyond the ovaries, influencing everything from weight and mood to skin, fertility, and long-term health risks.
In this guide, we’ll break down what PCOS really is, how it manifests, and the most effective treatment options based on current medical understanding.
What Is PCOS?
Polycystic Ovary Syndrome is a hormonal imbalance involving excess androgens (male hormones), irregular ovulation, and often the presence of multiple small cysts on the ovaries. These cysts are not harmful in themselves, but the hormonal disruption they represent can trigger a wide range of symptoms and health complications.
Importantly, you don’t need to have ovarian cysts to be diagnosed with PCOS. The diagnosis usually depends on meeting two of the following three criteria, known as the Rotterdam Criteria:
- Irregular or absent menstrual cycles
- Signs of high androgen levels (e.g., acne, facial hair, hair thinning)
- Polycystic ovaries visible on ultrasound
Common Symptoms of PCOS
The symptoms of PCOS vary significantly from person to person and can range in severity. Some women experience only mild disruptions, while others deal with more severe effects that impact both their physical and emotional well-being.
1. Irregular Periods
One of the hallmark signs of PCOS is a disrupted menstrual cycle. Women may have fewer than nine periods a year, very heavy bleeding, or no periods at all. This happens because the hormonal imbalance interferes with ovulation.
2. Excess Hair Growth (Hirsutism)
Elevated androgen levels lead to unwanted hair growth, especially on the face, chest, back, or abdomen. This can be particularly distressing for women and may require ongoing cosmetic treatment.
3. Acne and Oily Skin
Hormonal fluctuations, especially elevated testosterone, can cause persistent, cystic acne—often around the jawline, chest, and back.
4. Weight Gain or Difficulty Losing Weight
Up to 80% of women with PCOS struggle with insulin resistance, making it harder to maintain a healthy weight. Weight tends to accumulate around the abdomen, increasing the risk of metabolic conditions.
5. Hair Thinning
Ironically, while excess androgens cause unwanted hair growth in some areas, they also lead to thinning scalp hair or male-pattern baldness in others.
6. Fertility Issues
Due to irregular ovulation or lack of ovulation, PCOS is one of the leading causes of female infertility. However, many women with PCOS can still conceive with proper management.
7. Darkened Skin Patches
Some women develop dark, velvety patches of skin, particularly around the neck, groin, or under the breasts. This condition is called acanthosis nigricans and is often linked to insulin resistance.
8. Mood Swings and Depression
PCOS doesn’t just affect physical health; it can have a serious impact on mental well-being. Anxiety, mood swings, and depression are common, often worsened by body image struggles or hormonal fluctuations.
What Causes PCOS?
The exact cause of PCOS isn’t fully understood, but several factors appear to contribute:
1. Genetics
PCOS often runs in families. If your mother or sister has it, you’re more likely to develop it as well.
2. Insulin Resistance
Many women with PCOS produce too much insulin, which encourages the ovaries to produce more androgens. This disrupts ovulation and increases fat storage, creating a cycle that’s hard to break.
3. Inflammation
Chronic low-grade inflammation, common in people with PCOS, may contribute to higher androgen levels and metabolic complications.
Health Risks Associated with PCOS
PCOS is more than a reproductive issue—it can increase the risk of serious long-term health conditions, including:
- Type 2 diabetes
- High blood pressure
- High cholesterol
- Heart disease
- Endometrial cancer
- Sleep apnea
- Non-alcoholic fatty liver disease (NAFLD)
The good news? Early diagnosis and treatment can significantly reduce these risks.
Effective Treatments for PCOS
While there’s currently no “cure” for PCOS, it can be successfully managed through a combination of lifestyle changes, medications, and support. Treatment goals typically focus on relieving symptoms, improving fertility, reducing risks, and improving quality of life.
1. Lifestyle Changes
For many women, lifestyle adjustments are the first-line treatment—especially if symptoms are mild or moderate.
Diet
A low-glycemic index (GI) diet that stabilizes blood sugar levels can dramatically improve insulin sensitivity and hormone balance. Think whole grains, lean proteins, vegetables, fruits, and healthy fats.
Avoid:
- Processed carbs
- Sugary snacks and drinks
- Excess dairy (for some women)
Exercise
Regular physical activity improves insulin sensitivity, boosts mood, and helps regulate menstrual cycles. A mix of aerobic exercise, resistance training, and HIIT workouts is ideal.
Weight Management
Even modest weight loss (5–10% of total body weight) can significantly reduce PCOS symptoms and improve ovulation rates.
2. Medications
When lifestyle changes alone aren’t enough, medications may be prescribed to manage specific symptoms.
a. Birth Control Pills
Combination oral contraceptives are commonly used to:
- Regulate periods
- Reduce androgen levels
- Clear acne
- Control hirsutism
They’re not suitable for everyone, especially those with a history of blood clots or smoking.
b. Metformin
Originally used for type 2 diabetes, metformin helps improve insulin sensitivity and lower blood sugar levels. It may also help regulate cycles and promote weight loss in some women with PCOS.
c. Anti-Androgen Medications
Drugs like spironolactone can reduce male hormone effects like facial hair and acne. These are often used alongside birth control.
d. Fertility Treatments
For women trying to conceive:
- Clomiphene (Clomid) and letrozole are oral medications that stimulate ovulation.
- Gonadotropins or IVF may be considered if first-line treatments don’t work.
3. Supplements and Natural Approaches
Some women find symptom relief using evidence-supported supplements:
- Inositol (especially Myo-inositol and D-chiro-inositol): improves insulin sensitivity and promotes ovulation
- Vitamin D: deficiency is common in PCOS and affects hormone balance
- Omega-3 fatty acids: support inflammation and insulin control
- Cinnamon: may reduce insulin resistance in some studies
Always consult your doctor before adding supplements, especially if taking medications.
4. Mental Health Support
Mental health is often overlooked in PCOS treatment, but anxiety, depression, and low self-esteem are very common. Consider:
- Therapy or counseling
- Mindfulness practices
- Support groups (in-person or online)
Emotional support is crucial for coping with PCOS, especially when dealing with chronic symptoms, infertility, or body image challenges.
PCOS and Pregnancy: What You Should Know
Although PCOS can make getting pregnant more difficult, many women with PCOS conceive and have healthy pregnancies with proper care.
If you’re trying to get pregnant:
- Start with lifestyle changes and track your ovulation.
- Consult a fertility specialist if conception doesn’t occur after 6–12 months of trying.
- Consider medications or assisted reproductive technology (ART) if needed.
Managing weight, blood sugar, and hormones before and during pregnancy reduces the risk of complications such as gestational diabetes, preeclampsia, and preterm birth.
Final Thoughts: Living Well with PCOS
Living with PCOS can be frustrating, especially when symptoms affect your confidence, health, or fertility. But with awareness, consistent care, and support, you can take control of the condition instead of letting it control you.
Whether you’re newly diagnosed or have struggled for years, it’s never too late to make empowering changes. From nutrition and exercise to medication and mental health care, managing PCOS is a journey of self-care, patience, and persistence.
When to See a Doctor
If you suspect that you have PCOS, it’s important to consult a healthcare provider for a proper diagnosis. The earlier the condition is diagnosed, the sooner treatment can begin, helping to prevent complications. A doctor may perform blood tests to measure hormone levels, an ultrasound to check for ovarian cysts, and a physical exam to assess symptoms.
Conclusion
PCOS is a multifaceted condition that can affect many aspects of a woman’s health. Understanding the symptoms, seeking early diagnosis, and utilizing both medical treatments and lifestyle changes can greatly improve the quality of life for women with PCOS. Whether you are struggling with irregular periods, acne, weight gain, or infertility, there are options available to help you manage your symptoms and reduce the risk of long-term health complications.
If you have PCOS, it’s important to take a holistic approach to managing your health. This includes medical treatments, lifestyle changes, and natural remedies that can improve your well-being. Always consult a healthcare provider before starting any new treatments or supplements.
Explore more articles on PCOS management and health tips, and feel free to leave a comment sharing your experiences.
Frequently Asked Questions
1. Can I have PCOS even if I have regular periods?
Yes. While irregular periods are a common symptom, some women with PCOS have regular cycles but still experience hormonal imbalances, acne, or ovarian cysts. A medical evaluation is necessary for an accurate diagnosis.
2. Is PCOS a lifelong condition?
PCOS is a chronic condition, but symptoms can be managed effectively through lifestyle changes, medications, and proper care. Hormonal fluctuations may shift over time, especially during events like pregnancy or menopause.
3. Can I get pregnant if I have PCOS?
Yes. Many women with PCOS conceive naturally or with fertility support. Treatments such as ovulation-inducing medications, weight management, and IVF can significantly increase the chances of pregnancy.
4. What is the main cause of PCOS?
The exact cause is unknown, but genetics, insulin resistance, and inflammation play major roles in its development. These factors contribute to hormonal imbalances and irregular ovulation.
5. Can PCOS be cured completely?
There’s currently no cure, but PCOS can be managed effectively. A combination of healthy eating, regular exercise, medication (if needed), and regular monitoring can help keep symptoms under control.
6. Does losing weight help PCOS?
Yes. Even a modest weight loss of 5–10% can help regulate periods, reduce insulin resistance, lower androgen levels, and improve fertility outcomes.
7. What foods should I avoid if I have PCOS?
Try to limit:
- Processed carbs and sugary foods
- Refined grains
- High-sugar beverages
- Trans fats and processed snacks
Opt for whole foods that support blood sugar balance and hormone health.
8. Can birth control pills treat PCOS?
While birth control doesn’t “cure” PCOS, it can regulate menstrual cycles, reduce acne, and lower excess hair growth. It’s commonly used for symptom management in women not trying to conceive.
9. Is PCOS only a reproductive issue?
No. PCOS affects metabolic, hormonal, and mental health as well. It increases the risk of type 2 diabetes, high cholesterol, heart disease, and mood disorders.
10. Can PCOS go away after menopause?
Symptoms like irregular periods stop after menopause, but the metabolic and hormonal risks—like diabetes and heart disease—can persist. Continued care is important even after periods end.


Pingback: The Truth About Birth Control: What You Need to Know
Pingback: Bathing During Periods: Grandma’s Wisdom vs. Modern Health
Pingback: Hirsutism: Excessive Hair Growth in Women Causes & Impact
Pingback: Testosterone Deficiency in Women: Causes & Treatments Tips