Table of Contents
Introduction
Breast cancer is one of the most common types of cancer that affects women globally, yet many people are unaware of how to detect it early. Early detection of breast cancer can significantly increase the chances of successful treatment, and recognizing the early signs can make all the difference in achieving a positive prognosis. Regular self-exams, knowing when to consult a healthcare provider, and undergoing routine screenings are all critical steps toward ensuring better health outcomes. However, the importance of education regarding the signs and symptoms of breast cancer cannot be overstated, as many women are unsure of what specific changes to look for in their breasts.
This post aims to help you understand how to spot potential warning signs of breast cancer, the importance of regular self-exams, and when it is crucial to seek medical advice. If you’re concerned about your breast health or want to learn more about how to stay proactive, keep reading to discover how you can better monitor your health.
What Is Breast Cancer?
Breast cancer occurs when cells in the breast tissue begin to grow uncontrollably. These abnormal cells may form a lump or tumor and can spread to other parts of the body if left untreated. The development of breast cancer can happen in different forms, affecting both men and women, although it is far more common in women.
There are two primary types of breast cancer:
- Ductal Carcinoma in Situ (DCIS): This is a non-invasive form of cancer that is confined to the milk ducts and has not spread to surrounding tissue.
- Invasive Breast Cancer: This type of cancer begins in the milk ducts or lobules and then spreads to surrounding tissue or other parts of the body, potentially leading to metastatic cancer.
The key to improving the prognosis of breast cancer is early detection. Understanding the early signs and recognizing potential symptoms early on can increase the likelihood of successful treatment. It is vital to remember that not all breast changes indicate cancer, but regular monitoring is essential for overall breast health.
For a comprehensive overview of breast cancer types, prevention, and treatment options, you can refer to Mayo Clinic’s Breast Cancer Information.
Early Signs of Breast Cancer You Should Be Aware Of
Many women are unsure of what changes in their breast tissue should concern them. While some breast changes are benign, being aware of specific symptoms and seeking medical advice when necessary is crucial for your health. Here are some key signs to watch out for:
1. A Lump in the Breast
A lump or mass in the breast is one of the most common signs of breast cancer. This lump is often painless, but it can vary in size and texture. It may feel firm or hard, and it’s important to pay attention to any changes in consistency.
Tip: If the lump feels irregularly shaped or hard, it’s crucial to visit your doctor for further testing. While many breast lumps are benign, such as those caused by cysts or fibrocystic changes, any new lump should be evaluated by a healthcare provider to rule out cancer.
2. Changes in Breast Shape or Size
Noticing any changes in the size or shape of one breast compared to the other is another early sign of breast cancer. One breast may become noticeably larger, swollen, or asymmetric compared to the other. This can be an indication that there may be an underlying issue, especially if the change is sudden or significant.
3. Skin Changes on the Breast
Breast cancer can cause changes in the skin of your breast, including:
- Redness: The skin may appear red or inflamed.
- Dimpling or puckering: The skin may resemble the texture of orange peel (peau d’orange), which is a sign of inflammatory breast cancer.
- Rash or flaky skin on the nipple: This can occur with certain types of breast cancer, particularly inflammatory breast cancer, which requires immediate medical attention.
Tip: If you notice any of these skin changes, it’s essential to contact a healthcare provider promptly for further evaluation.
4. Pain or Tenderness in the Breast
Pain in the breast is not typically associated with early-stage breast cancer, but some women do experience tenderness or discomfort in the breast or nipple area. If the pain persists and does not correspond to your menstrual cycle or any known causes, it is important to discuss it with your doctor.
5. Nipple Discharge
Unusual discharge from the nipple, particularly if it is clear, bloody, or milky, can be an early sign of breast cancer. While some discharge can be normal (such as during breastfeeding), any spontaneous or abnormal discharge, especially blood-stained, should be evaluated by a doctor.
6. Swelling or Lumps in the Armpit
Swelling or lumps in the underarm area (also called axillary lymph nodes) can be a sign that cancer has spread to nearby lymph nodes. This often occurs in the early stages of invasive breast cancer. If you notice any lumps in the armpit or swelling, it’s important to seek medical attention.
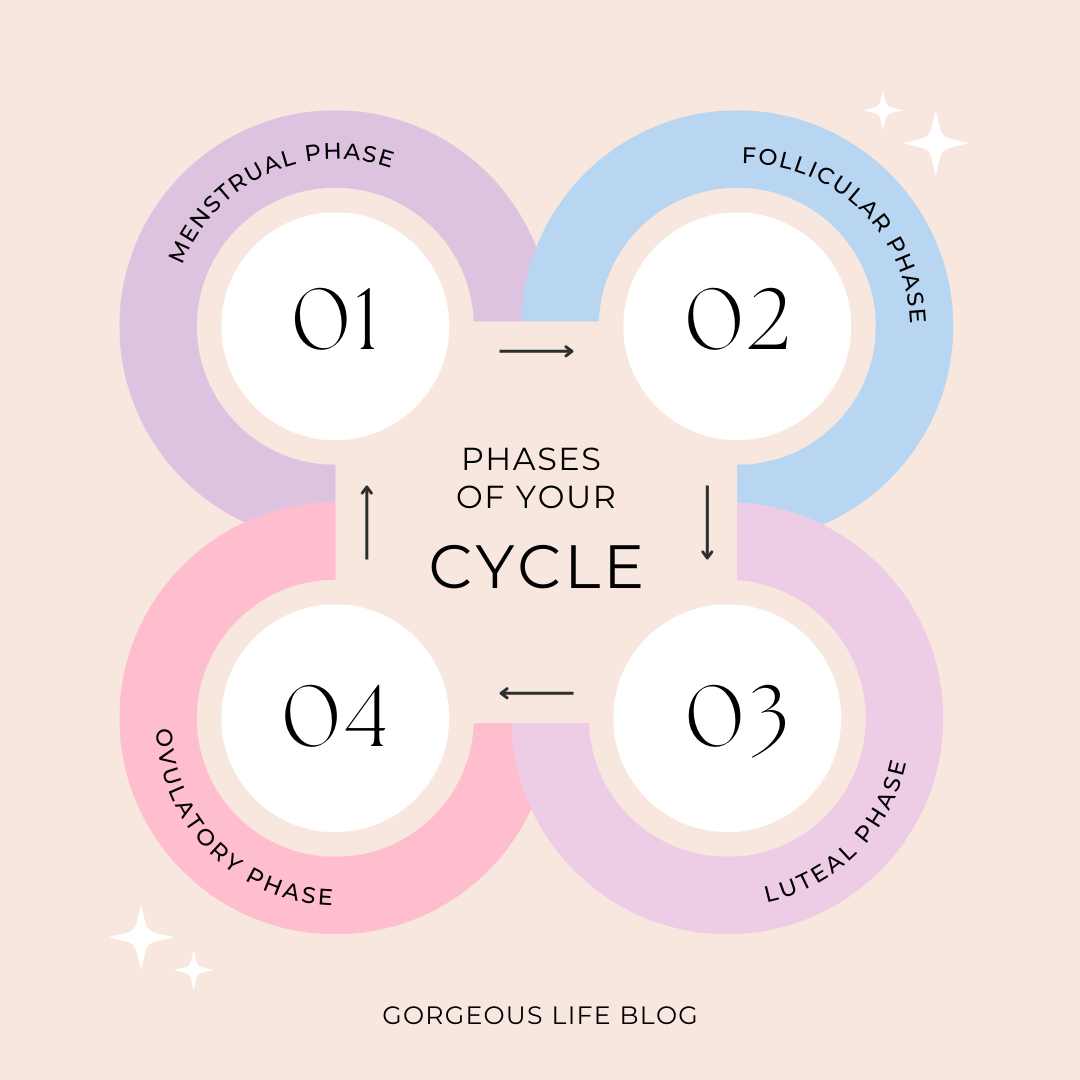
Understanding the Link Between Hormonal Changes and Breast Cancer Risk
Hormonal changes can have a significant influence on breast cancer development. Estrogen and progesterone, the key hormones involved in the menstrual cycle, can stimulate breast tissue, and prolonged exposure to these hormones can increase the risk of breast cancer.
Hormonal fluctuations during perimenopause and menopause can also play a role in altering the breast tissue and potentially increasing the risk of breast cancer. Women with higher levels of estrogen over time may face a higher risk, especially if they have a family history of breast cancer.
If you’re experiencing hormonal imbalances or undergoing hormonal treatments, it’s essential to monitor any changes in your breast health. Hormonal shifts can sometimes lead to changes in breast tissue that require medical evaluation.
For more detailed information on hormonal health and its impact on breast cancer risk, read about hormonal changes and mental health to understand the broader implications.
Why Early Detection of Breast Cancer Is So Important
Early detection of breast cancer increases the chances of successful treatment. When breast cancer is detected early, it is more likely to be localized to the breast, which makes it easier to treat with less aggressive approaches. The earlier the detection, the less likely the cancer is to have spread to other parts of the body.
Regular screenings such as mammograms and self-exams are the most effective tools for detecting breast cancer early. Women should discuss with their healthcare provider when to begin regular mammograms based on their individual health history and risk factors. Women with a family history of breast cancer may need to start screenings earlier than the general population.
For more information on breast cancer prevention and screening guidelines, visit Healthline’s Breast Cancer Guide.
The Role of Regular Self-Exams
One of the most effective ways to stay proactive about your breast health is through regular breast self-exams. By performing a self-exam monthly, you become more familiar with the normal texture and appearance of your breasts. This familiarity will allow you to notice any unusual changes that may indicate a potential issue.
How to Perform a Breast Self-Exam:
- Positioning: Stand in front of a mirror with your arms raised. Look for any changes in the shape, size, or appearance of your breasts, paying attention to any skin changes, dimpling, or abnormal lumps.
- Using Your Fingers: While standing or lying down, use the pads of your fingers to move in small, circular motions across your breasts, feeling for any lumps, thickening, or changes in texture. Be sure to check all areas of your breasts, including the upper chest and underarms.
- Check for Lumps or Discharge: Gently squeeze each nipple to check for any discharge. Examine all areas, including the armpits, collarbone, and around the breast tissue.
- Repeat Monthly: Perform your self-exam at the same time each month, ideally about a week after your period ends, when your breasts are least likely to be swollen or tender.
To learn more about how to perform breast self-exams, visit Mayo Clinic’s Self-Examination Guide.
When to See a Doctor
If you notice any of the symptoms mentioned above, or if you’re unsure about changes you’ve observed, it’s essential to seek medical advice. In many cases, the changes may be benign (non-cancerous), but only a healthcare provider can make an accurate diagnosis. If you notice any of the following, schedule an appointment with your doctor:
- A lump that persists for more than a few weeks
- Changes in size or shape of your breast
- Redness, dimpling, or puckering of the skin on your breast
- Unusual nipple discharge
- Pain that is constant and unrelated to your menstrual cycle
Diagnostic tests such as mammograms, ultrasounds, and biopsies will help confirm whether the changes are cancerous or benign. The earlier you seek medical advice, the better your chances of successful treatment.
Diagnostic Tests for Breast Cancer
If a doctor suspects breast cancer, they may recommend several tests to confirm the diagnosis. These tests include:
- Mammogram: A mammogram is an X-ray of the breast that can detect tumors or abnormal tissue before they can be felt. It is an essential tool for early breast cancer screening.
- Ultrasound: Ultrasound imaging uses sound waves to produce pictures of the inside of your breast. It can help distinguish between solid masses and fluid-filled cysts, which may be non-cancerous.
- Biopsy: If a suspicious lump is found, a biopsy may be performed to remove a small tissue sample. This sample is examined under a microscope to determine if it contains cancer cells.
For further information on breast cancer testing, visit WebMD’s Breast Cancer Diagnosis.
External Resources
For more information on breast cancer detection, treatment options, and preventive measures, check out these trusted resources:
- Healthline’s Guide to Breast Cancer: Healthline’s Breast Cancer Information
- Mayo Clinic’s Breast Cancer Information: Mayo Clinic’s Breast Cancer Overview
Conclusion: Stay Vigilant and Prioritize Your Health
Breast cancer remains a significant health concern, but recognizing early signs and acting promptly can substantially improve treatment outcomes. Regular self-exams, understanding warning signs, and consulting healthcare providers when necessary are crucial steps in maintaining breast health. Additionally, it’s important to be aware of conditions like Polycystic Ovary Syndrome (PCOS), which can impact hormonal balance and overall well-being.
By staying informed and proactive, you can better safeguard your health and well-being. Regular monitoring and screenings are essential for every woman, particularly as they approach the recommended screening age or if they have a family history of breast cancer.
For more information on managing hormonal health and understanding conditions like PCOS, consider exploring this comprehensive guide on PCOS: Understanding Symptoms & Effective Treatment. This resource provides valuable insights into recognizing symptoms and exploring treatment options for PCOS, empowering you to take charge of your health.
For more health tips and information, explore our other articles or leave a comment below with any questions.
Frequently Asked Questions About Breast Cancer
1. What are the early signs of breast cancer?
- Early signs of breast cancer can include a lump in the breast, changes in breast shape or size, skin changes such as redness or dimpling, persistent pain or tenderness, unusual nipple discharge (especially if it’s clear, bloody, or milky), and swelling or lumps in the armpit area. It’s important to note that not all of these symptoms are cancerous, but they should be evaluated by a healthcare provider.
2. How often should I perform a breast self-exam?
- It’s recommended to perform a breast self-exam once a month, ideally about a week after your period ends, when your breast tissue is least likely to be swollen or tender. If you’re post-menopausal, choose a specific day of the month to perform your self-exam consistently.
3. Are breast self-exams effective in detecting breast cancer?
- Yes, performing regular breast self-exams is an important step in detecting early signs of breast cancer. By becoming familiar with your breasts, you will be able to identify any unusual changes more quickly. However, self-exams should complement regular mammograms and doctor visits, not replace them.
4. What is the role of mammograms in breast cancer detection?
- Mammograms are X-ray images of the breast that can detect tumors or abnormalities even before they can be felt. Regular mammograms are one of the most effective ways to catch breast cancer early, often when it is most treatable. Women over 40 are typically advised to have mammograms every year, but those with a family history of breast cancer may need to start earlier.
5. Can men get breast cancer?
- Yes, although breast cancer is much more common in women, men can also develop breast cancer. Men have a small amount of breast tissue where cancer can form, though it is rare. Men should be aware of any lumps, changes in breast tissue, or nipple discharge and consult a healthcare provider if they notice any unusual signs.
6. What factors increase the risk of breast cancer?
- Several factors can increase the risk of breast cancer, including a family history of the disease, age (risk increases with age), hormonal factors (early menstruation or late menopause), personal history of breast cancer or certain non-cancerous breast diseases, and exposure to estrogen through hormone replacement therapy or certain birth control methods.
7. How does family history impact the risk of breast cancer?
- A family history of breast cancer, especially in a first-degree relative (mother, sister, or daughter), can significantly increase your risk. Certain genetic mutations, such as BRCA1 and BRCA2, also contribute to a higher risk of developing breast cancer. If you have a family history, it’s essential to discuss early screening options with your doctor.
8. What are the treatment options for breast cancer?
- Treatment for breast cancer can vary based on the stage and type of cancer. Common treatments include surgery (to remove the tumor), chemotherapy (to destroy cancer cells), radiation therapy (to target cancer cells), hormone therapy (to block hormones that fuel cancer growth), and targeted therapies (which attack specific cancer cells). Your healthcare provider will work with you to develop a personalized treatment plan based on the specific characteristics of your cancer.
9. How does hormonal therapy work in breast cancer treatment?
- Hormonal therapy works by blocking or lowering the amount of hormones, particularly estrogen and progesterone, that fuel some types of breast cancer. This therapy is typically used for estrogen-receptor-positive breast cancers and can help reduce the risk of cancer recurrence. It may involve medications like tamoxifen or aromatase inhibitors.
10. Is breast cancer preventable?
- While breast cancer cannot always be prevented, there are steps you can take to reduce your risk. These include maintaining a healthy diet and weight, exercising regularly, limiting alcohol consumption, avoiding smoking, and considering the use of hormone replacement therapy cautiously. If you have a family history or high-risk factors, your doctor may suggest additional preventive measures like medications or prophylactic surgery.
11. How can I reduce my risk of breast cancer?
- To reduce the risk of breast cancer, maintain a healthy lifestyle by eating a balanced diet, staying physically active, and avoiding excessive alcohol and tobacco use. Regular screenings, such as mammograms, and being aware of any changes in your breast tissue are important. Additionally, maintaining a healthy weight and considering options like breastfeeding can also contribute to lowering your risk.
12. What are the survival rates for breast cancer?
- The survival rates for breast cancer have greatly improved due to advances in early detection and treatment. The five-year survival rate for women with localized breast cancer (cancer that has not spread) is around 99%. The survival rate decreases if the cancer has spread to other parts of the body, but early detection remains the key to improving outcomes.
13. Can I still live a full life after a breast cancer diagnosis?
- Yes, many people live full, healthy lives after being diagnosed with breast cancer. Advances in treatment have made it possible for people to continue their normal activities and enjoy a good quality of life after treatment. Emotional support, regular follow-up care, and lifestyle adjustments are also essential to help manage life after breast cancer.
14. What role does exercise play in breast cancer prevention and recovery?
- Exercise plays a vital role in both breast cancer prevention and recovery. Studies have shown that regular physical activity can lower the risk of breast cancer, particularly in postmenopausal women. After treatment, exercise can help improve overall health, boost energy levels, reduce stress, and aid in the recovery process by improving strength and stamina.
15. Is breast cancer hereditary?
- Breast cancer can be hereditary, but most cases are not. Only 5–10% of breast cancer cases are inherited due to specific gene mutations like BRCA1 or BRCA2. If you have a family history of breast cancer or know that your family carries these mutations, it’s important to discuss genetic testing and early screening options with your healthcare provider.



Pingback: The Importance of Breast Health: Key Tips To Aware