Table of Contents
Introduction
Women’s health is deeply influenced by a variety of complex microbiomes, particularly the vaginal and endometrial microbiomes. Research into the microbial communities that populate these areas is expanding, revealing their role in everything from fertility to the regulation of immune responses. These microbiomes are not just passive passengers but active players in maintaining health and influencing disease processes. The relationship between the microbiome and reproductive health is increasingly recognized as pivotal, offering new insights into how microbial imbalances may contribute to various health challenges women face. Let’s break down what we know so far and why this is important.
Understanding the vaginal and endometrial microbiomes is essential for advancing our understanding of women’s reproductive health. These microbiomes are complex ecosystems, and their balance or imbalance can profoundly impact health outcomes such as fertility, pregnancy, and even the risk of developing certain diseases.
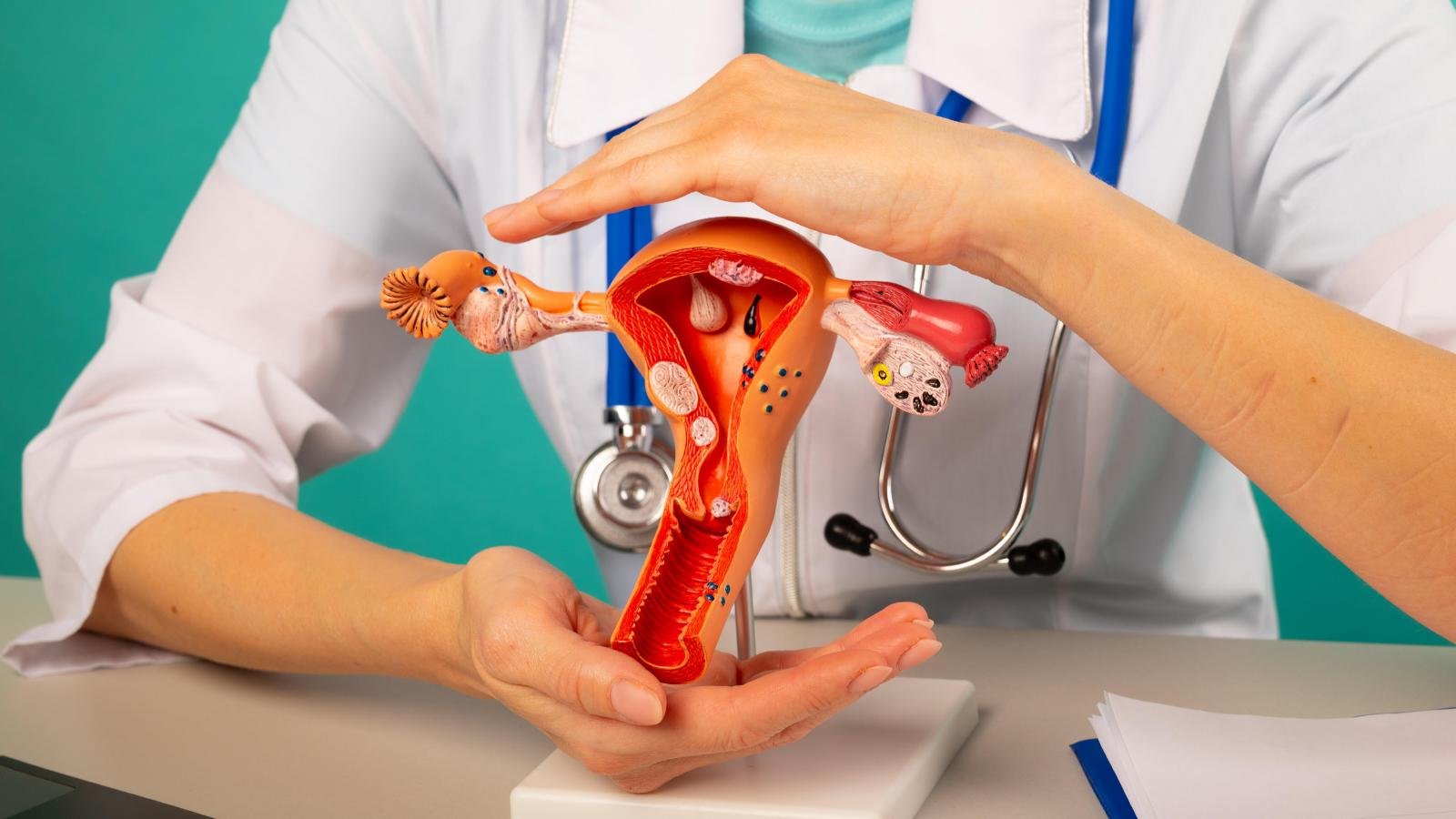
Understanding the Vaginal Microbiome
The vaginal microbiome refers to the diverse population of microorganisms that reside in the vaginal canal. It is a delicate ecosystem, primarily dominated by bacteria, including Lactobacillus species. These bacteria are crucial because they help maintain an acidic environment, which protects against harmful pathogens. The predominance of Lactobacillus species helps keep the vaginal pH between 3.8 and 4.5, which creates a hostile environment for many harmful microbes.
When this microbiome is balanced, it plays a critical role in preventing infections, such as bacterial vaginosis (BV) and yeast infections, which can disrupt vaginal health. A healthy vaginal microbiome supports the body’s immune system and helps maintain overall well-being.
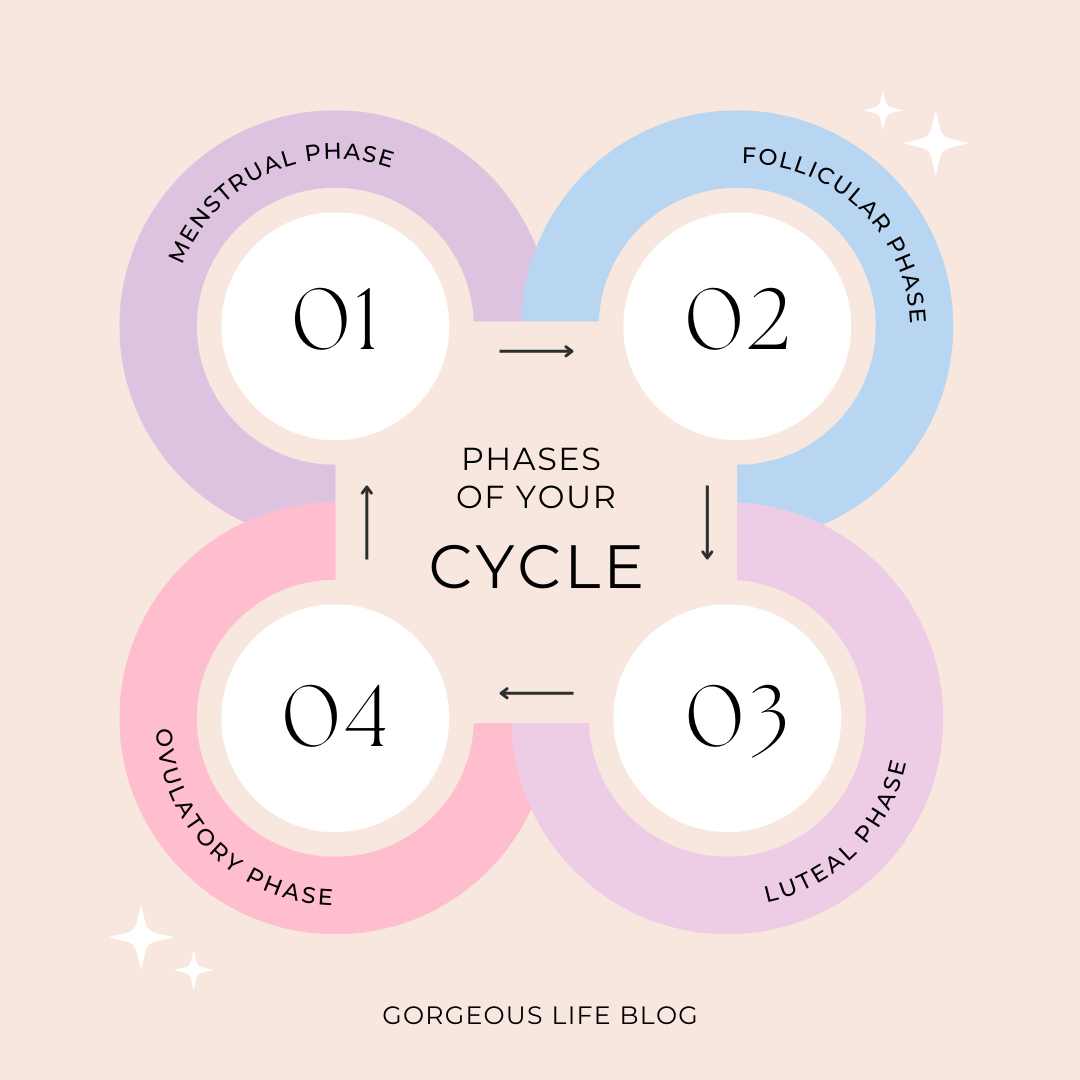
However, the vaginal microbiome isn’t static. It changes over time due to several factors, including hormonal fluctuations, sexual activity, menstrual cycles, and the use of antibiotics. This dynamic nature means the vaginal microbiome is highly susceptible to disruptions, which can lead to a variety of health issues, including increased susceptibility to sexually transmitted infections (STIs) and vaginal dryness.
Recent studies suggest that the vaginal microbiome may also influence reproductive health. For example, women with an imbalanced vaginal microbiome have been found to have a higher risk of infertility, miscarriage, and complications during pregnancy. Research indicates that an imbalance in vaginal microbiota can impact sperm motility and their ability to fertilize an egg. Additionally, a healthy vaginal microbiome is believed to facilitate implantation and reduce the risk of preterm birth.
What this really means is that the vaginal microbiome plays an essential role in the initial stages of conception and pregnancy. This has profound implications for how we approach fertility and reproductive health. This growing body of research may offer new insights into treating reproductive health issues and improving outcomes for women struggling with infertility.
The Endometrial Microbiome: A New Frontier
Until recently, it was believed that the uterus was a sterile environment. However, emerging evidence shows that the endometrium—the lining of the uterus—also hosts a distinct microbiome. This discovery is still relatively recent, and research is ongoing to understand the full scope of its impact. Researchers have now identified that microbial communities in the endometrial environment can influence fertility, pregnancy outcomes, and even the risk of conditions like endometriosis and other reproductive disorders.
The endometrial microbiome is influenced by the vaginal microbiome, but it has its own unique composition. Lactobacillus species still play a dominant role in the endometrium, but there are significant differences in microbial populations between the vagina and the uterus. In healthy women, the endometrial microbiome is typically diverse and balanced. However, disruptions in the microbiome—such as an overgrowth of pathogenic bacteria—have been linked to infertility, recurrent miscarriage, and abnormal pregnancy outcomes.
Studies have shown that a healthy endometrial microbiome promotes an ideal environment for embryo implantation. Conversely, an imbalance in the microbiome may lead to chronic inflammation or immune system dysfunction, which can impede embryo attachment and lead to miscarriage. Research is still in its early stages, but these findings highlight how crucial the endometrial microbiome may be for women’s reproductive health.
Implications for Fertility and Reproductive Health
The vaginal and endometrial microbiomes are now recognized as crucial factors in fertility and reproductive health. When these microbiomes are out of balance, it’s not just an inconvenience—it can have significant consequences on a woman’s ability to conceive and maintain a pregnancy. Several key factors contribute to this, including the following:
Microbial Imbalance and Infertility
The relationship between microbial balance in the vagina and endometrium and fertility is becoming clearer. Disruptions in the vaginal microbiome—such as an overgrowth of Gardnerella, Atopobium, or Mobiluncus—can lead to bacterial vaginosis, which is associated with delayed conception and increased risk of miscarriage. Additionally, research has found that the microbiomes in the cervix and uterus may affect sperm motility, sperm DNA integrity, and the likelihood of successful fertilization.
For instance, imbalances in the vaginal microbiome can alter the environment in the cervix, making it more difficult for sperm to survive and swim toward the egg. Additionally, imbalances in the uterine microbiome may make it harder for an embryo to implant successfully, leading to implantation failure or miscarriage.
The Role of Inflammation
An imbalanced microbiome can trigger chronic inflammation, which is detrimental to fertility. Inflammatory cytokines can disrupt the normal function of reproductive tissues and hinder implantation. Chronic low-grade inflammation, often observed in conditions like endometriosis, can lead to a hostile environment for embryo implantation.
The endometrial microbiome plays a vital role in regulating immune responses and ensuring the proper inflammatory environment for embryo implantation. A disrupted microbiome may lead to immune system dysfunction, chronic inflammation, and, ultimately, failure to conceive or maintain a pregnancy.
Preterm Birth and Pregnancy Complications
The vaginal microbiome may also impact pregnancy outcomes. Imbalances in the microbiome have been linked to a higher risk of preterm birth. Studies show that a healthy vaginal microbiome helps maintain a balanced immune response during pregnancy, reducing the risk of infections and complications. Women with a disrupted vaginal microbiome, particularly those with low levels of Lactobacillus, are more susceptible to infections that can increase the risk of preterm labor.
For more information on how the vaginal microbiome affects pregnancy outcomes, visit Mayo Clinic’s Guide on Pregnancy Complications.
Cervicovaginal Microbiome and IVF Success
There’s growing interest in how the vaginal and endometrial microbiomes may affect assisted reproductive technologies, like in vitro fertilization (IVF). Some studies suggest that an optimal microbiome may increase the likelihood of successful embryo implantation, while a dysbiotic microbiome may lead to implantation failure. Research is still needed to establish concrete connections, but the findings so far are promising.
IVF success rates could potentially be improved by optimizing the vaginal and endometrial microbiomes before and during the IVF process. This opens up new avenues for research and treatment in reproductive medicine.
The Impact of Lifestyle and Diet
What’s fascinating about the vaginal and endometrial microbiomes is that they aren’t entirely determined by genetics. Environmental factors—such as lifestyle, diet, and medication use—play a significant role in shaping the microbial populations in these areas. Understanding how lifestyle influences the microbiome can help women make informed choices about their health and fertility.
Diet and Probiotics
Studies have shown that a diet rich in fiber, prebiotics, and fermented foods can positively influence the gut, vaginal, and endometrial microbiomes. Foods high in fiber promote the growth of beneficial bacteria, while probiotics (found in foods like yogurt, kefir, and kimchi) can help replenish Lactobacillus populations, which are crucial for maintaining balance in the vaginal microbiome.
Additionally, certain foods have been shown to reduce inflammation in the body, which is important for maintaining a healthy microbiome. Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, have anti-inflammatory properties that support a balanced immune system and microbiome.
Antibiotic Use
The widespread use of antibiotics is another critical factor influencing microbial health. While antibiotics are effective in fighting infections, they can also wipe out beneficial bacteria, leading to imbalances in both the gut and vaginal microbiomes. Studies have shown that antibiotic use can increase the risk of BV, yeast infections, and even pelvic inflammatory disease (PID), all of which can impact fertility.
To maintain a healthy microbiome, it’s essential to use antibiotics judiciously and follow your doctor’s advice regarding treatment options.
Sexual Activity and Hygiene Practices
Sexual activity and hygiene practices also influence microbiome health. Engaging in protected sex can help prevent the transmission of sexually transmitted infections (STIs), which can disrupt the vaginal microbiome. Additionally, maintaining proper hygiene without over-washing or using harsh chemicals can support the natural balance of the microbiome.
Exercise and Physical Activity
Physical activity also plays a significant role in supporting a healthy microbiome. Regular exercise can reduce stress, promote blood circulation, and improve immune function, all of which contribute to a healthier microbiome. Understanding the connection between exercise and the microbiome is still an area of active research, but some studies suggest that moderate exercise may increase the diversity of beneficial gut bacteria, which could indirectly support reproductive health.
For more insights on balancing your fitness routine with your body’s natural rhythms, consider learning more about cycle syncing workouts, which align exercise with different phases of your menstrual cycle.
Future Directions in Microbiome Research
Despite the promising findings, there’s still a lot to learn about the vaginal and endometrial microbiomes. The field is in its infancy, and much of the research is still observational. As we move forward, there are several key areas that need further exploration:
Microbiome and Disease Prevention
Understanding how the vaginal and endometrial microbiomes influence diseases like endometriosis, PID, and even cervical cancer could lead to new preventive strategies. Research suggests that a healthy microbiome may help protect against these conditions by maintaining a balanced immune response and preventing harmful infections.
Microbiome Restoration and Fertility Treatments
If an imbalance in the vaginal or endometrial microbiome is found to be contributing to infertility, interventions could be developed to restore balance. Probiotics, prebiotics, and dietary changes may offer potential solutions, but more clinical trials are needed to determine the most effective methods for restoring microbiome health in women with fertility issues.
Personalized Medicine and Microbiome Profiling
With advancements in microbiome sequencing, we may soon be able to offer personalized treatments based on an individual’s microbiome profile. This could revolutionize the way we approach fertility treatments and women’s health.
Conclusion
The vaginal and endometrial microbiomes are integral to women’s health, particularly in relation to fertility and pregnancy. As research into these microbiomes progresses, it is becoming clear that maintaining a balanced microbial community is crucial for optimal reproductive outcomes. While we’re still learning about the full scope of their impact, one thing is certain: the future of women’s reproductive health will likely be deeply intertwined with the health of these microbiomes.
To stay ahead, we must continue exploring how lifestyle, diet, and targeted treatments can help support a healthy microbiome. By taking proactive steps to support the microbiome through proper diet, exercise, and mindful health practices, women can improve their fertility and overall reproductive health. Additionally, maintaining a healthy weight and focusing on sustainable weight loss methods, such as those outlined in Lose Weight Fast Without Starving: Proven Strategies, can help improve overall health, which may, in turn, support microbiome balance.
For further information on women’s health and microbiome research, consider checking out more of our health articles and resources.
Frequently Asked Questions About the Vaginal and Endometrial Microbiomes
1. What is the vaginal microbiome?
- The vaginal microbiome refers to the community of microorganisms that live in the vaginal canal. It is primarily composed of bacteria, including Lactobacillus species, which help maintain an acidic environment that protects against harmful pathogens. A balanced vaginal microbiome is crucial for preventing infections and promoting vaginal health.
2. How does the vaginal microbiome affect fertility?
- A balanced vaginal microbiome plays an important role in fertility. An imbalanced microbiome can impact sperm motility, DNA integrity, and the ability to fertilize an egg. It also facilitates embryo implantation and reduces the risk of preterm birth. Disruptions in the vaginal microbiome are associated with higher risks of infertility, miscarriage, and complications during pregnancy.
3. What factors can disrupt the vaginal microbiome?
- Several factors can disrupt the vaginal microbiome, including hormonal changes (e.g., during menstruation, pregnancy, or menopause), antibiotic use, sexual activity, and hygiene practices. An imbalanced diet or excessive use of certain medications can also affect microbial populations in the vaginal area.
4. What is the endometrial microbiome?
- The endometrial microbiome refers to the microbial community that resides in the lining of the uterus (endometrium). It was once believed that the uterus was sterile, but recent research has shown that it also hosts a distinct microbiome, which plays a role in fertility and pregnancy outcomes. An imbalance in the endometrial microbiome has been linked to conditions such as infertility, recurrent miscarriage, and complications during pregnancy.
5. How does the endometrial microbiome influence fertility?
- The endometrial microbiome influences fertility by promoting a healthy environment for embryo implantation. When the microbiome is in balance, it supports immune regulation, reduces inflammation, and ensures a favorable environment for successful embryo attachment. Disruptions in the microbiome can lead to inflammation or immune dysfunction, which may impair embryo implantation and increase the risk of miscarriage.
6. Can diet affect the vaginal and endometrial microbiomes?
- Yes, diet plays a significant role in shaping both the vaginal and endometrial microbiomes. A diet rich in fiber, prebiotics, and fermented foods can promote the growth of beneficial bacteria, while foods high in sugar and processed fats may contribute to microbial imbalances. Probiotics (found in foods like yogurt, kimchi, and kefir) can help replenish beneficial bacteria, including Lactobacillus species, which are important for maintaining microbiome balance.
7. How do antibiotics impact the vaginal microbiome?
- Antibiotics are often necessary to treat infections, but they can also disrupt the vaginal microbiome by killing both harmful and beneficial bacteria. This disruption can lead to imbalances that increase the risk of conditions like bacterial vaginosis (BV) or yeast infections. It’s essential to use antibiotics judiciously and consider probiotics to restore balance after antibiotic treatment.
8. Can exercise improve the vaginal and endometrial microbiomes?
- Regular physical activity can positively influence the vaginal and endometrial microbiomes by reducing stress, improving immune function, and promoting overall health. Moderate exercise has been shown to enhance microbiome diversity and may improve the balance of beneficial bacteria. Additionally, cycle syncing workouts, which tailor exercise routines to the different phases of a woman’s menstrual cycle, can help optimize hormonal balance and microbiome health.
9. What role does the vaginal microbiome play in pregnancy?
- A healthy vaginal microbiome is essential for a healthy pregnancy. It helps regulate the immune system and prevents infections that could lead to complications, such as preterm birth. Women with a disrupted vaginal microbiome are at a higher risk of developing infections, which can affect pregnancy outcomes. Ensuring a balanced vaginal microbiome may improve the chances of carrying a pregnancy to term.
10. Can a disrupted microbiome affect IVF success?
- Research is ongoing, but some studies suggest that an optimal vaginal and endometrial microbiome may improve the chances of successful embryo implantation during in vitro fertilization (IVF). A dysbiotic microbiome could reduce the likelihood of implantation or lead to IVF failure. As the science evolves, further studies may reveal more concrete evidence about how microbiomes affect assisted reproductive technologies.
11. What can I do to maintain a healthy vaginal and endometrial microbiome?
- To maintain a healthy vaginal and endometrial microbiome, focus on lifestyle habits that promote microbial balance. This includes eating a balanced diet with fiber, prebiotics, and probiotics, managing stress, avoiding excessive antibiotic use, and practicing safe sex. Regular physical activity, good hygiene practices, and mindfulness around medication use can also support microbiome health.
12. Can lifestyle changes improve my fertility if my microbiome is out of balance?
- Yes, lifestyle changes such as improving your diet, reducing stress, and incorporating exercise can help restore balance to your vaginal and endometrial microbiomes, potentially improving fertility. Probiotic supplements, along with foods that encourage the growth of beneficial bacteria, may also help. If you suspect microbiome imbalances are affecting your fertility, it’s important to consult a healthcare provider for further testing and treatment.
13. Is there a test to check the health of my vaginal or endometrial microbiome?
- While research is still in its early stages, some tests are available that can analyze the vaginal microbiome to detect imbalances. These tests are often used in clinical research but may also be available through some healthcare providers. Similarly, as more is learned about the endometrial microbiome, there may be diagnostic tests in the future that assess its composition. Currently, diagnosing microbiome imbalances typically involves evaluating symptoms and conducting other relevant tests, such as swabs or imaging.
14. How does the microbiome affect other reproductive health conditions?
- The microbiome is increasingly recognized as playing a role in various reproductive health conditions, including endometriosis, pelvic inflammatory disease (PID), and polycystic ovary syndrome (PCOS). An imbalance in the microbiome can exacerbate symptoms of these conditions by promoting chronic inflammation, disrupting immune responses, or affecting hormone regulation. Understanding the microbiome’s role may open new pathways for treatments and interventions.
15. Can probiotics improve the health of my vaginal microbiome?
- Yes, probiotics can help replenish beneficial bacteria, such as Lactobacillus, in the vaginal microbiome. Probiotic supplements or probiotic-rich foods like yogurt, kefir, and fermented vegetables can support a healthy balance of vaginal bacteria. However, it’s important to consult with a healthcare provider before starting any new supplements, especially if you’re dealing with an existing condition like bacterial vaginosis or yeast infections.
External Resources
For further reading on the vaginal and endometrial microbiomes, as well as general women’s health, explore the following trusted health resources:
- Healthline’s Guide to Vaginal Health: Healthline Vaginal Health
- Mayo Clinic’s Guide on Fertility: Mayo Clinic Fertility Information


Pingback: Lupus and Women’s Health: Managing the Chronic Disease